Colorectal cancer: introduction
What is colorectal cancer?
There are several types of large bowel cancer and they are named after the cells that they develop from. Adenocarcinomas are the most common type of large bowel cancer. These tumours start in the lining of internal layer of the bowel. Other types of malignant tumours in the large bowel (such as lymphoma or carcinoid) are rather rare. These tumours are treated in another way than adenocarcinomas, and they often have other symptoms, too. This information is mainly about adenocarcinoma of the large bowel and rectum. Colon cancer and rectal cancer have a lot in common, and they are often referred to as colorectal cancer. However, there are some differences, particularly as regards their treatment.
What are the symptoms of colorectal cancer?
Colorectal cancer can have a variety of symptoms, although these might be almost imperceptible at very early stages of the disease.
- A change in your normal bowel habit for no obvious reason, lasting longer than six weeks, should not be ignored. It can be diarrhoea or constipation, a feeling of not having emptied your bowel properly after a bowel motion, or difficult emptying. Thin or ribbon-like stools may be a symptom of advanced colorectal cancer.
- Bleeding from the rectum or blood in the stools – the blood may be bright red or dark in colour – is another warning sign.
- Slow, chronic blood loss within the body – such as from a colorectal cancer – can cause iron deficiency anaemia. Its symptoms may involve fatigue and weakness, sometimes also dyspnoea.
- General abdominal discomfort, such as frequent gas pains, bloating, and/or cramps might also be symptoms of colorectal cancer.
- Weight loss with no known reason might also be linked to colorectal cancer.
- As colon cancer grows, several symptoms may appear. Bowel obstruction may produce symptoms of abdominal distension, pain, nausea, and vomiting.
It is important to bear in mind that all of the above-mentioned symptoms can be caused by non-malignant and less serious conditions. In particular, these involve haemorrhoids, infectious and inflammatory bowel diseases. However, colorectal cancer can develop over a long period without any symptoms, and manifest itself at an advanced stage of the disease. In case of any doubts, it is essential to see a GP, who should make arrangements for all necessary examinations.
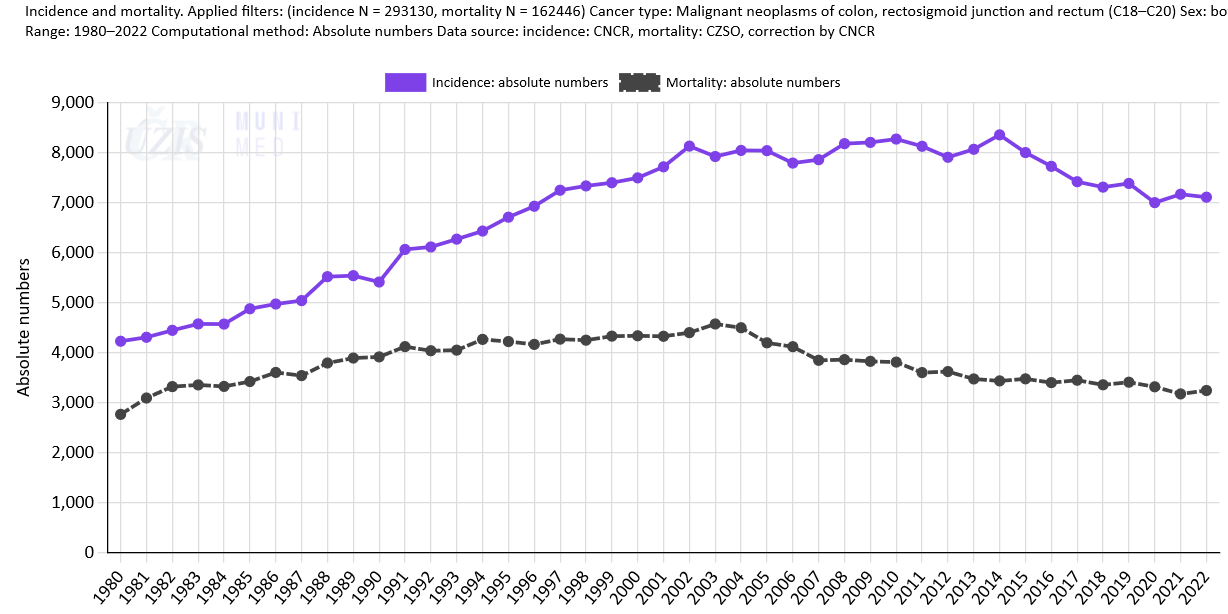
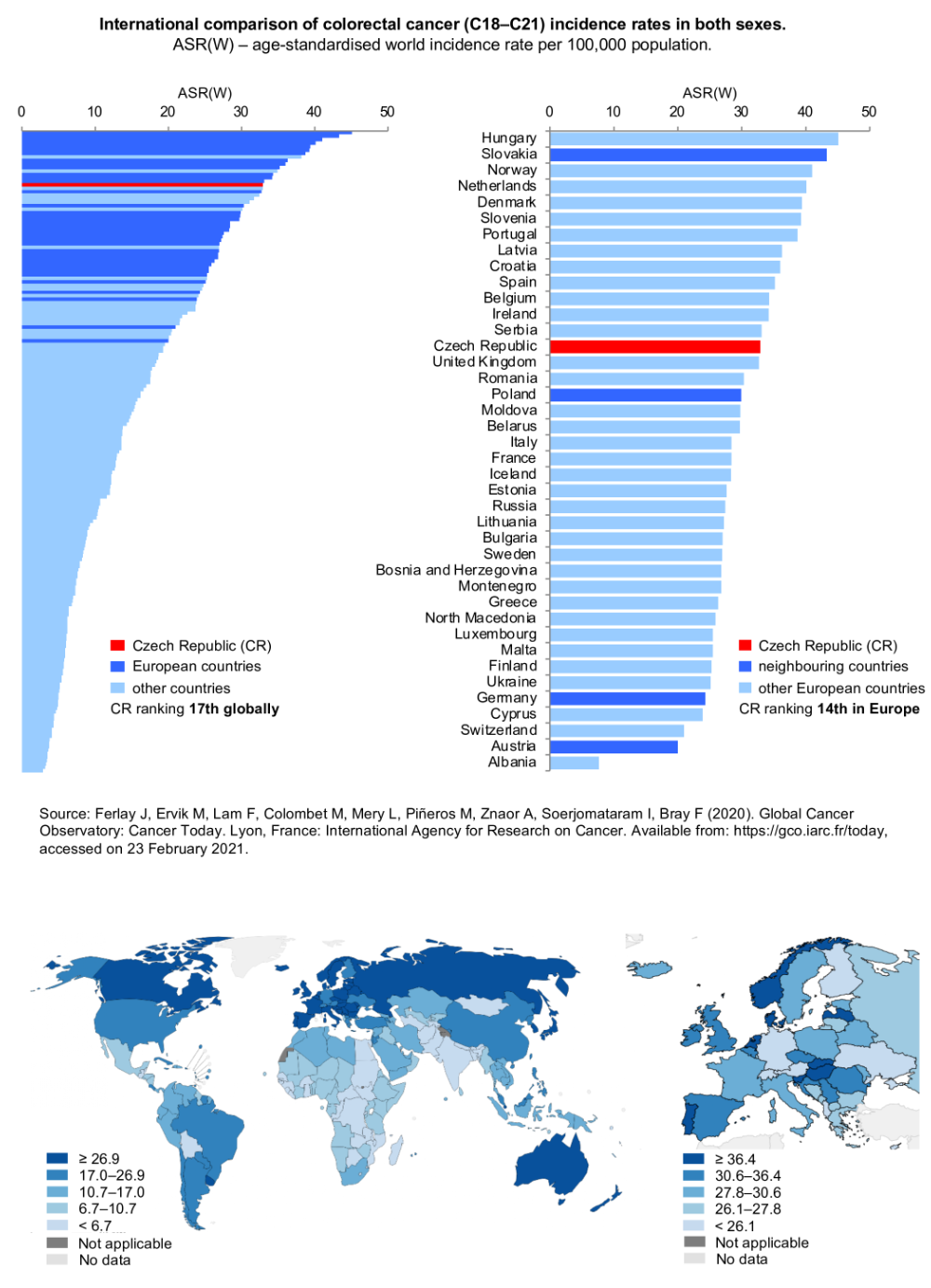
Incidence of colorectal cancer in the Czech Republic
Colorectal cancer (CRC) is among the most commonly diagnosed cancers and its incidence rates in all developed countries are growing steadily. In international comparison, the burden of colorectal cancer in the Czech Republic is comparable to that in European countries on average. According to data from 2018, Czech male colorectal cancer incidence rates rank 14th in Europe, while female rates rank 19th in Europe. Each year around 7,200 patients are diagnosed with colorectal cancer in the Czech Republic, and the number of CRC deaths is almost 3,300.
More detailed information on colorectal cancer in the Czech Republic is available in the article Colorectal cancer: epidemiology and screening results.
Colorectal cancer prevention and risk factors
The occurrence of colorectal cancer can be largely prevented by primary and secondary prevention. Read more in the article Cancer prevention. The exact cause of colorectal cancer is unknown in most patients. However, there are some risk factors known to increase the risk of developing colorectal cancer.
Age
Age is one risk factor for colorectal cancer. Colorectal cancer most typically occurs in people aged 45 and above, but can also affect younger people.
Colon polyps
Some types of polyps present another risk factors. Polyps are outgrowths from the intestinal wall. After a long time, some of these polyps give rise to carcinoma. It is therefore necessary to remove all polyps from the colon and rectum and to examine them carefully, just to make sure that they are really polyps and not carcinomas. Polyps can recur and therefore might need to be removed repeatedly.
Genetic predisposition
Genetic predisposition is also important for the development of colorectal cancer. The risk is higher if colorectal cancer occured in first-degree relatives, i.e. in parents, siblings or children. In some cases, the genetic disorder is so characteristic that colorectal cancer will almost certainly develop at some time in the future. These conditions involve, for example, the familial adenomatous polyposis (FAP).
Inflammatory bowel disease (IBD)
Some diseases, such as ulcerative colitis or Crohn’s disease, also increase the risk of developing colorectal cancer.
Dietary habits
Dietary habits play a significant role in health and mortality, and can be easily influenced, as opposed to many other risk factors. An excessive consumption of animal fats, red meat and processed meats has a definitely negative impact on our health, and significantly increases the risk of developing colorectal cancer. Energy-dense foods (foods high in fats and/or added sugars and/or low in fibre) are high in fats sugars and can be low in nutrients. These foods, especially when consumed frequently or in large portions, increase the risk of obesity, which in turn increases the risk of cancer. Furthermore, evidence shows that vegetables, fruits and other foods containing dietary fibre (such as wholegrains and pulses) may protect against a range of cancers including mouth, stomach and bowel cancer.
How is colorectal cancer diagnosed?
If a bowel tumour is suspected, the doctor will take a medical history by interviewing the patient. In the medical history, the doctor asks, for example, whether there is a history of cancer in the patient’s family, what the problems are and for how long they have been observed, whether there has been any sudden weight loss, any abdominal pain or blood in the stool, any constipation or diarrhoea.
During the actual examination, the doctor will carefully palpate the abdomen. A digital rectal examination is an important part of the examination. This simple examination can sometimes reveal a tumour in the rectum.
A variety of different examination methods are used in the diagnosis of colorectal cancer (e.g. colonoscopy, abdominal ultrasound, abdominal CT scan, magnetic resonance imaging and laboratory blood tests). The doctor decides on the appropriate combination of these according to the individual patient’s condition.
How is colorectal cancer treated?
First of all, it is important to understand that colorectal cancer is a treatable disease! Therefore, there is no need to despair, no matter how unpleasant the news of cancer is. Especially the early stages of the disease can be treated very well and the patient has a great hope for a long and good life.
The treatment of colorectal cancer includes surgical treatment, chemotherapy, radiation therapy (radiotherapy), and targeted cancer therapies with monoclonal antibodies. Interventional radiological methods have seen great development. A combination of these treatment methods is often necessary.
Knowledge of the extent of the cancer is necessary before deciding on treatment, so it is necessary to undergo the necessary examinations.
Before starting any treatment, the patient should be informed about the treatment plan and possible different treatment options. Sufficient information should also be provided about the possible risks and side effects of cancer treatment.
Supportive therapy is also an essential part of cancer treatment. The aim of supportive therapy is to manage possible side effects of cancer therapy, such as nausea and vomiting, infections and possible other complications. Supportive therapy also deals with the management of complications that accompany the cancer itself – for example, pain management.