Colorectal cancer: epidemiology and screening results
Czech Republic
The Czech National Cancer Registry (CNCR) is the main source of data on cancer epidemiology in the Czech Republic. CNCR has become an integral part of comprehensive cancer care, containing more than 3 million records from the period 1977–2022 and covering 100% of the Czech population. Registration of malignant tumours is stipulated by law and is obligatory [1]. CNCR data is publicly available on the website www.svod.cz [2].
-
Colorectal cancer incidence and mortality rates
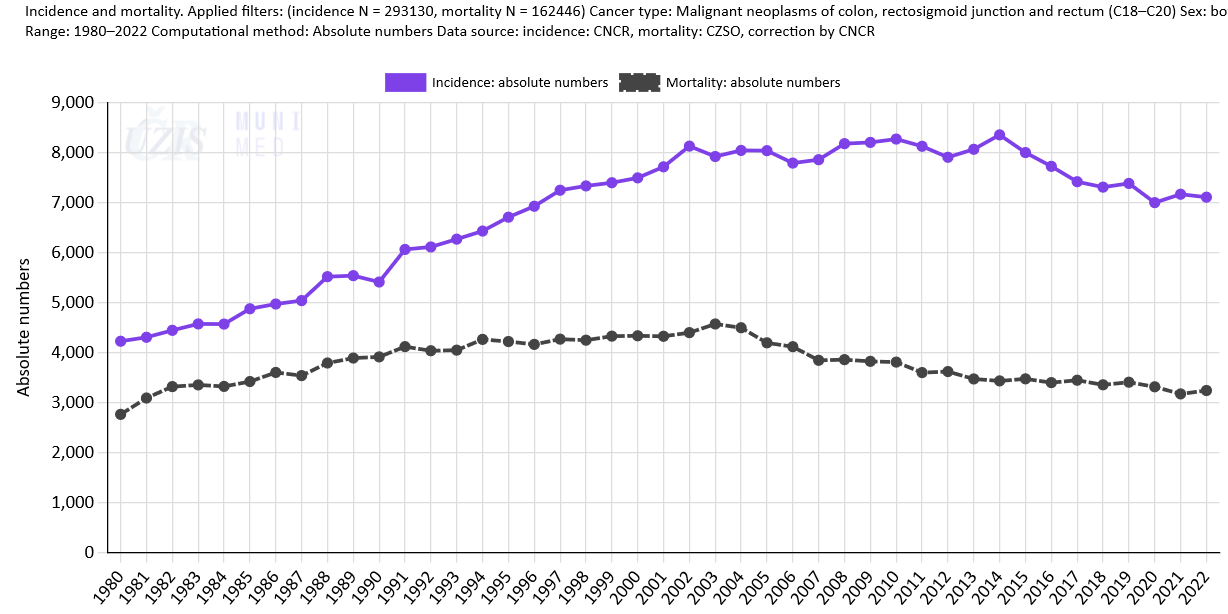
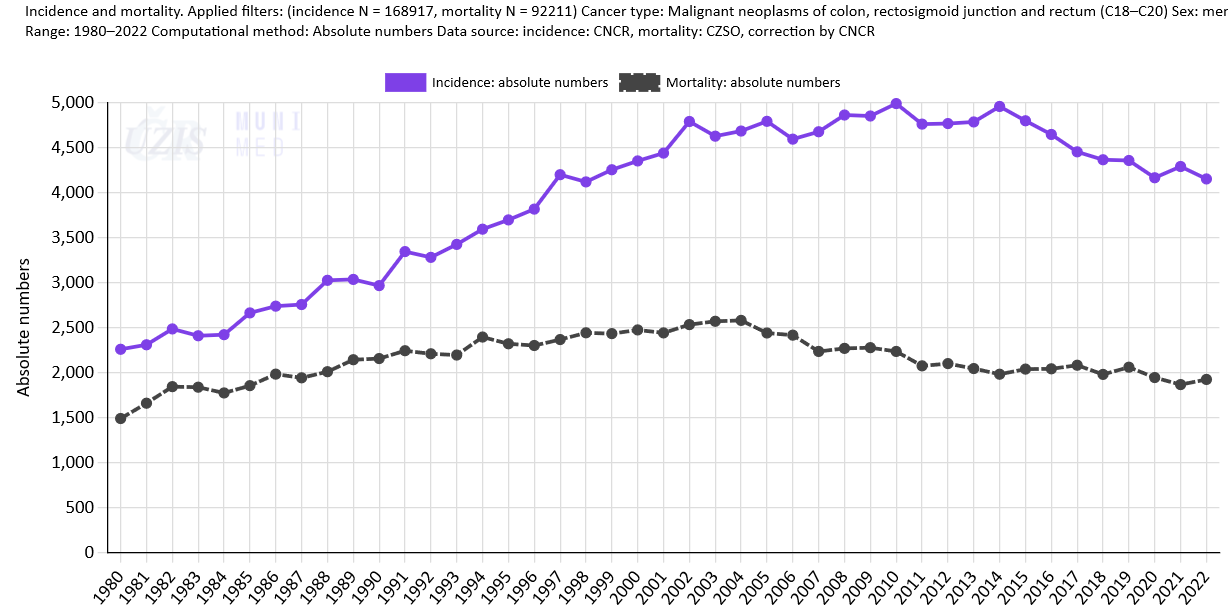
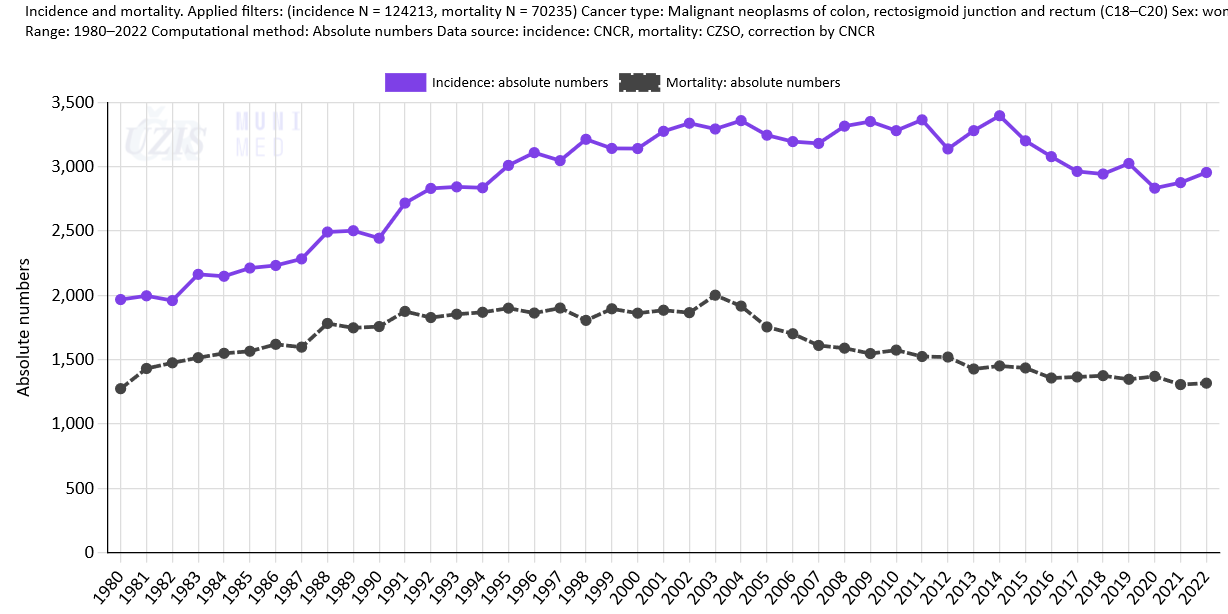
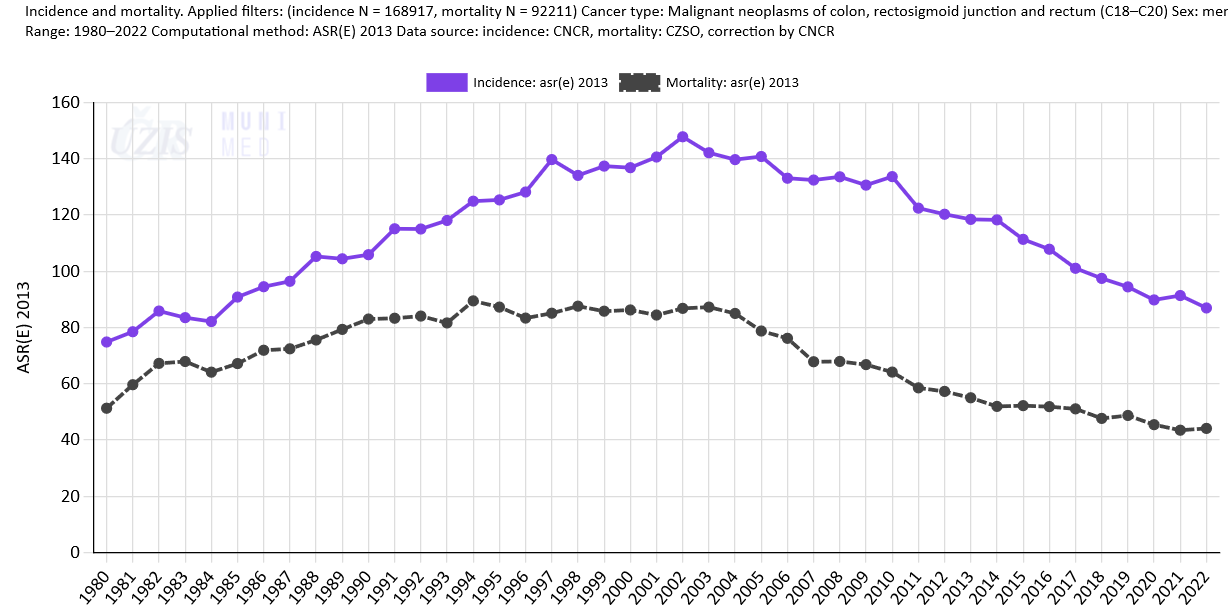
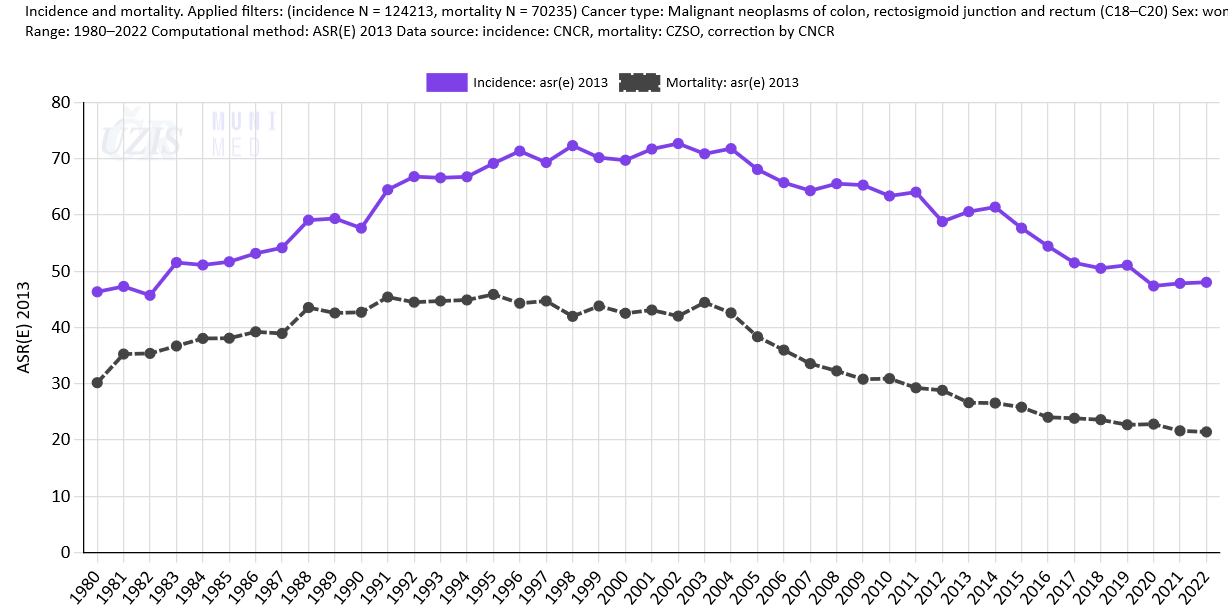
Colorectal cancer (CRC) is among the most commonly diagnosed cancers and its incidence rates in all developed countries are growing steadily. In international comparison, the burden of colorectal cancer in the Czech Republic is comparable to that in European countries on average. According to the latest data from GLOBOCAN 2018 [3], Czech male colorectal cancer incidence rates rank 14th in Europe, while female rates rank 19th in Europe (see more details in Epidemiology of colorectal cancer: International comparison). The population burden is very high indeed: each year around 7,200 patients are diagnosed with colorectal cancer in the Czech Republic, and there are approximately 3,300 deaths from colorectal cancer among the Czech population (Fig. 1a). Both incidence and mortality rates for colorectal cancer are higher in men than in women (Figs. 1b, 1c).
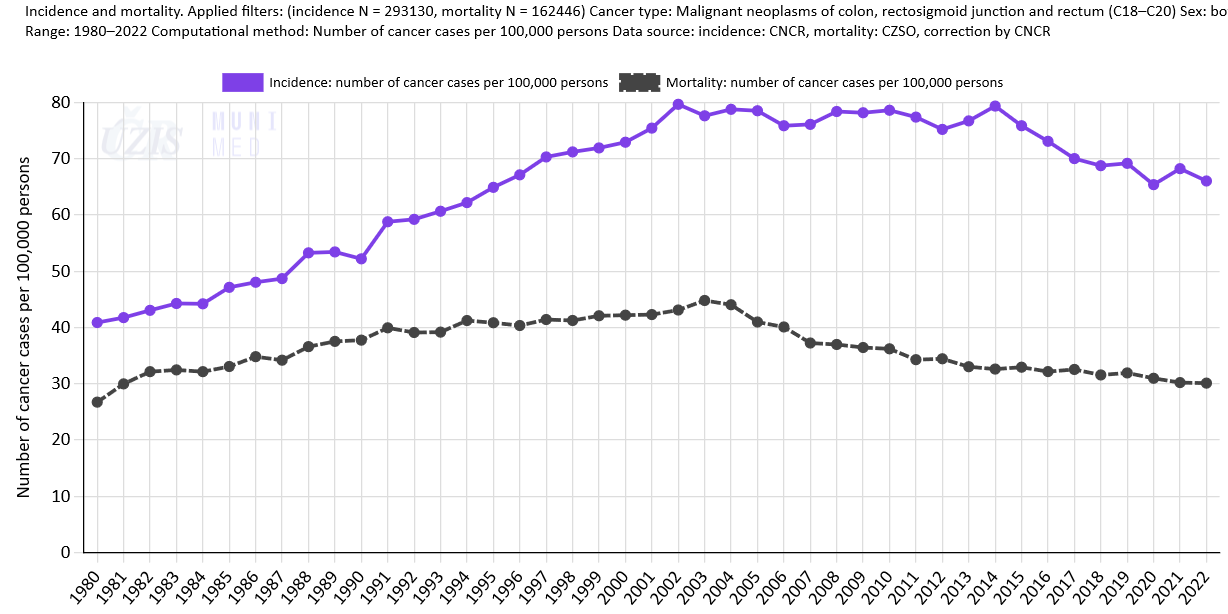
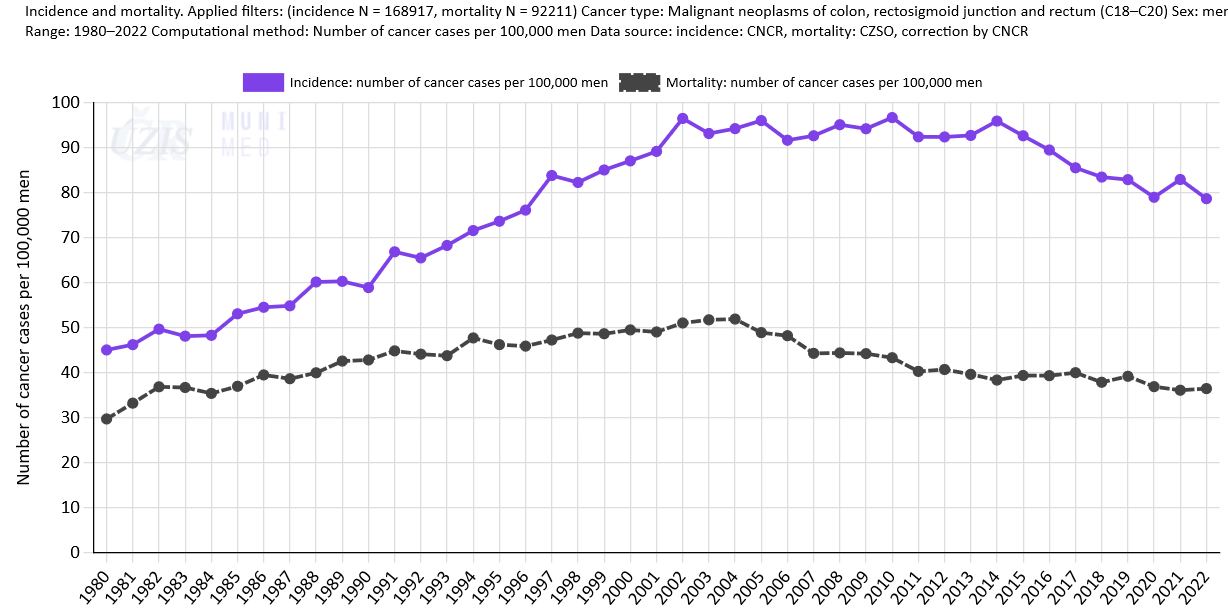
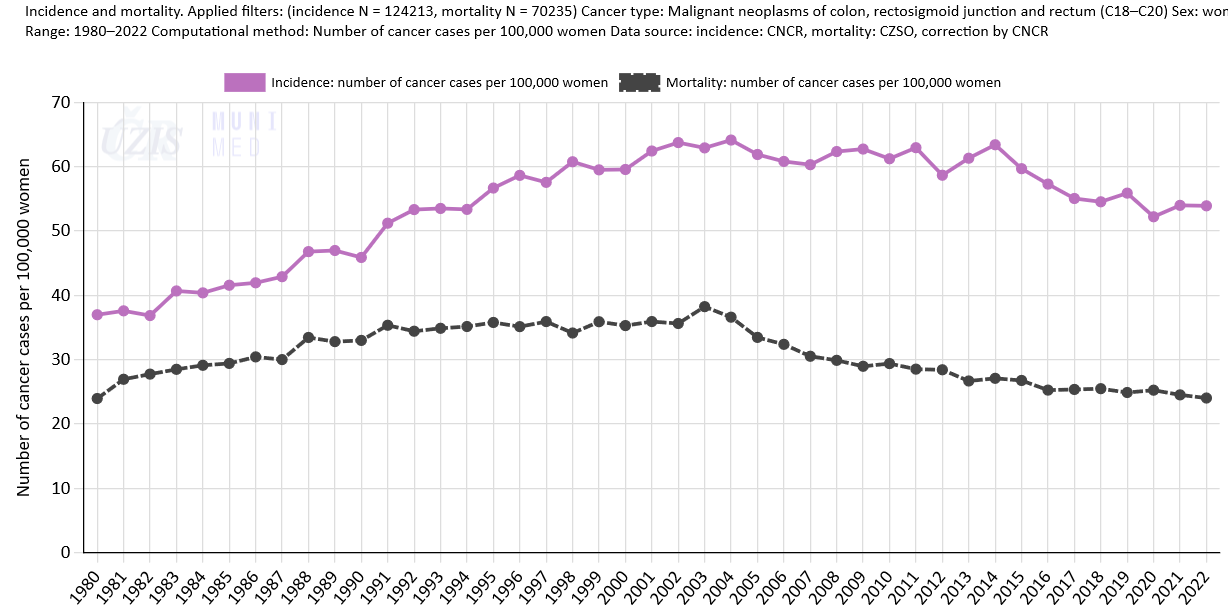
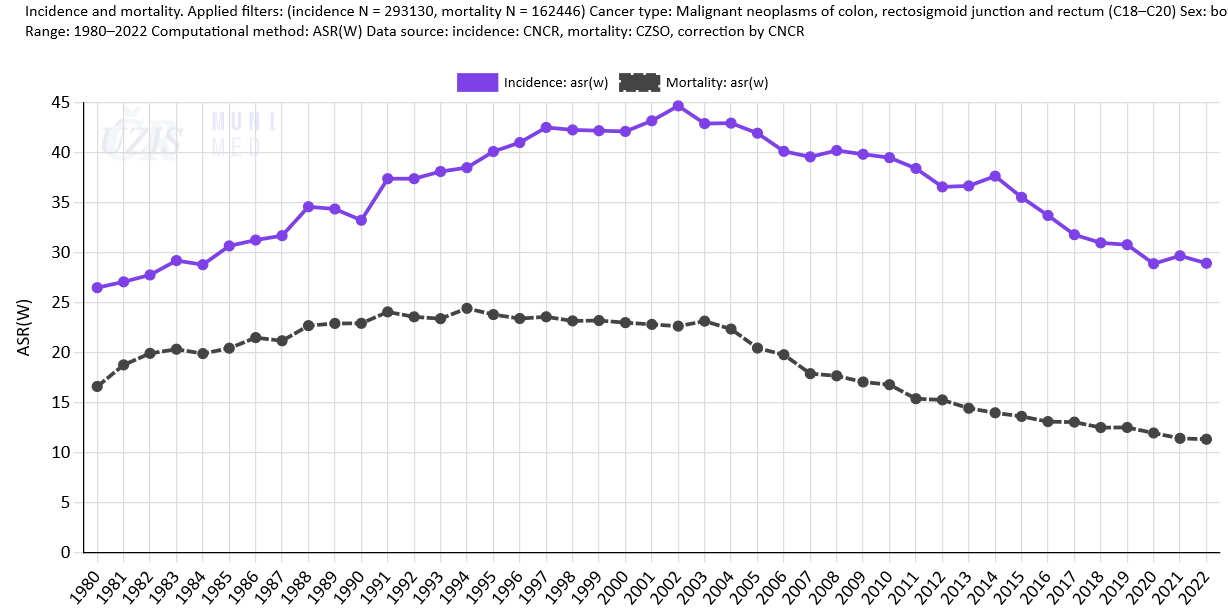
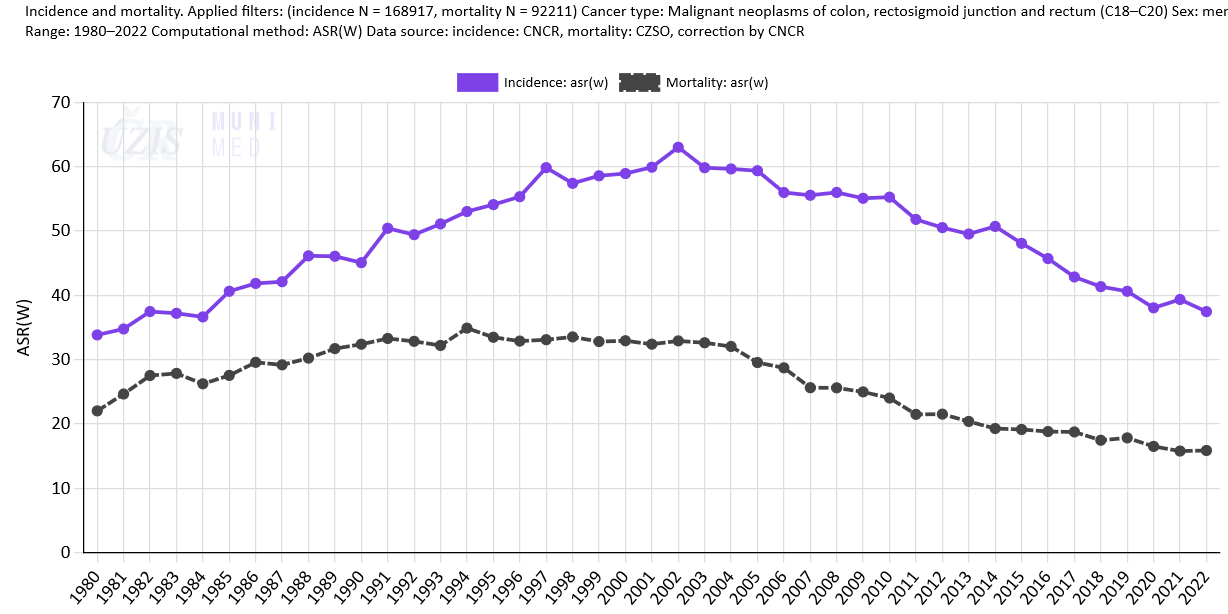
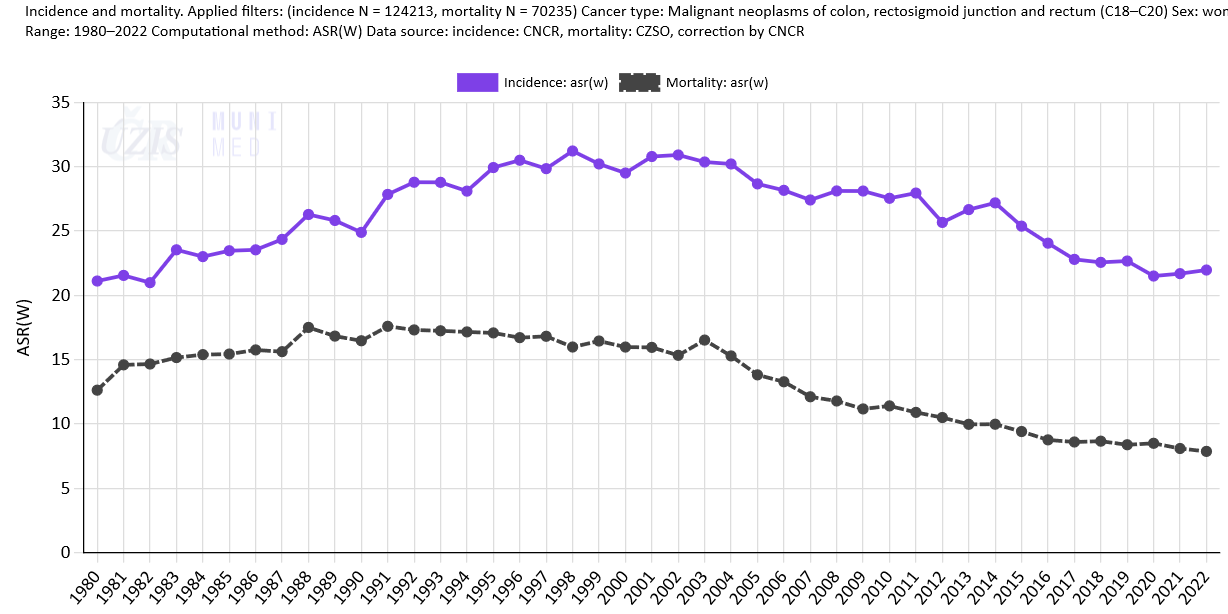
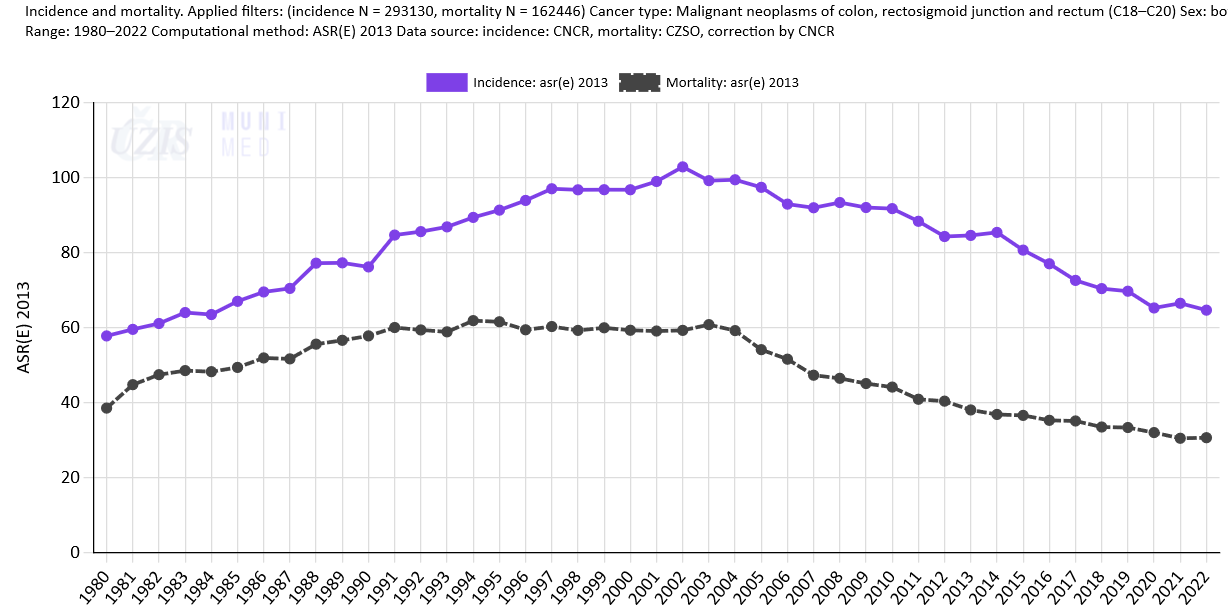
Apart from absolute numbers of newly diagnosed cases and deaths per year (Figs. 1a-c), CRC incidence and mortality rates can be recalculated per 100,000 persons (or men, women) in the population (Figs. 2a-c) or standardised on a certain age standard; the most common ones include the age-standardised world rate (ASR-W, Figs. 3a-c) and the new age-standardiseded European rate (ASR-E 2013, Figs. 4a-c). Such recalculations make it possible to compare CRC incidence and mortality rates with those of other countries (see more details in Epidemiology of colorectal cancer: International comparison).
Absolute numbers of new cases / deaths
Figure 1a: C18–C20 incidence and mortality, both sexes. Data source: CNCR (incidence in the entire period, mortality up to 1993), CZSO (mortality since 1994)
Figure 1b: C18–C20 incidence and mortality, men. Data source: CNCR (incidence in the entire period, mortality up to 1993), CZSO (mortality since 1994)
Rates per 100,000 persons
Figure 2a: C18–C20 incidence and mortality, both sexes. Data source: CNCR (incidence in the entire period, mortality up to 1993), CZSO (mortality since 1994)
Figure 2b: C18–C20 incidence and mortality, men. Data source: CNCR (incidence in the entire period, mortality up to 1993), CZSO (mortality since 1994)
Age-standardised world rates (ASR-W)
Figure 3a: C18–C20 incidence and mortality (ASR-W), both sexes. Data source: CNCR (incidence in the entire period, mortality up to 1993), CZSO (mortality since 1994)
Figure 3b: C18–C20 incidence and mortality (ASR-W), men. Data source: CNCR (incidence in the entire period, mortality up to 1993), CZSO (mortality since 1994)
Age-standardised European rates (ASR-E)
Figure 4a: C18–C20 incidence and mortality (ASR-E), both sexes. Data source: CNCR (incidence in the entire period, mortality up to 1993), CZSO (mortality since 1994)
Figure 4b: C18–C20 incidence and mortality (ASR-E), men. Data source: CNCR (incidence in the entire period, mortality up to 1993), CZSO (mortality since 1994)
-
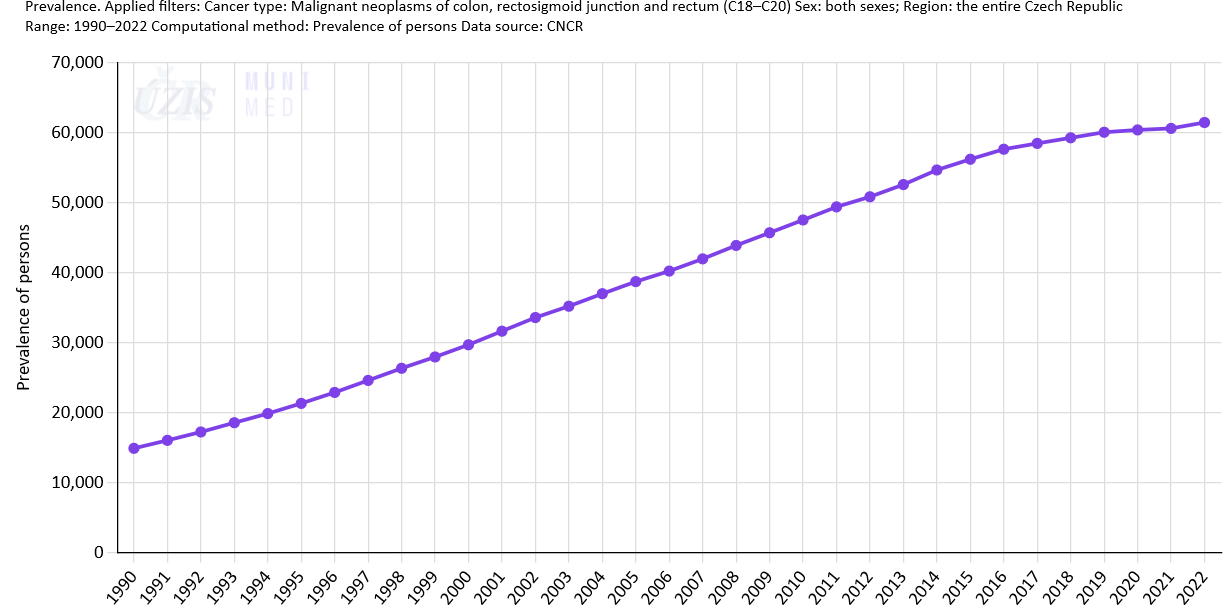
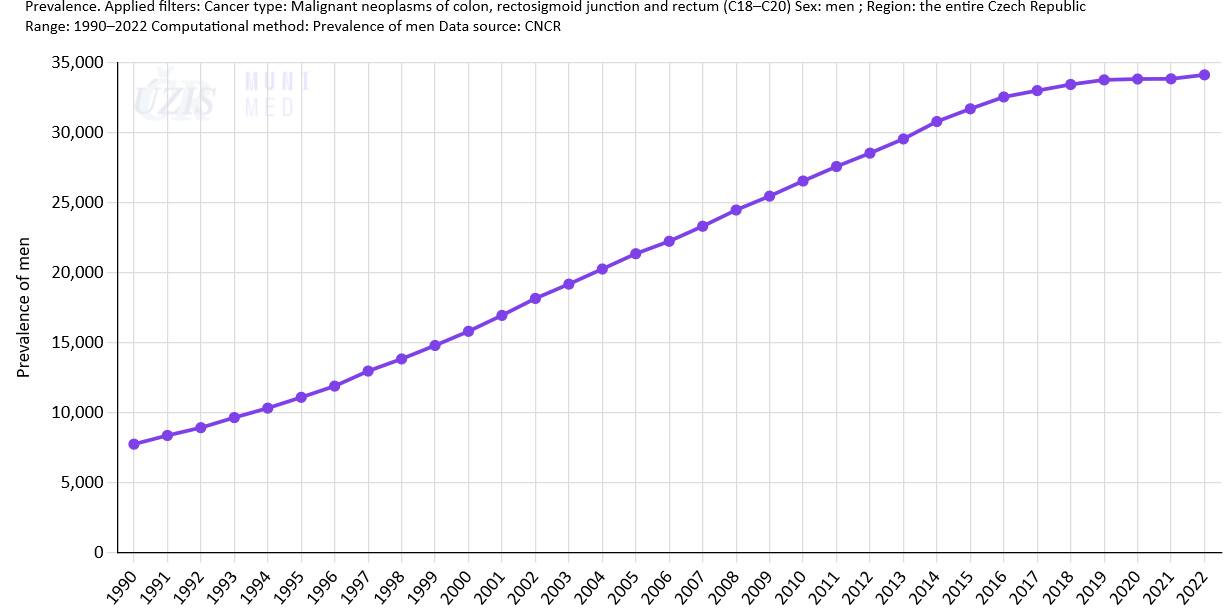
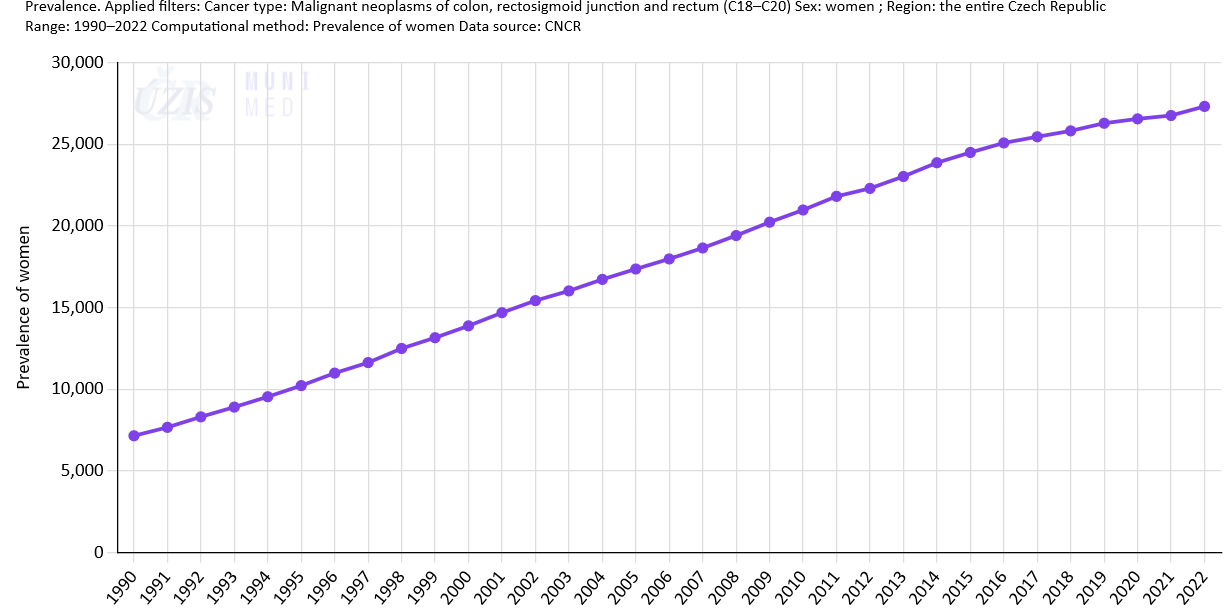
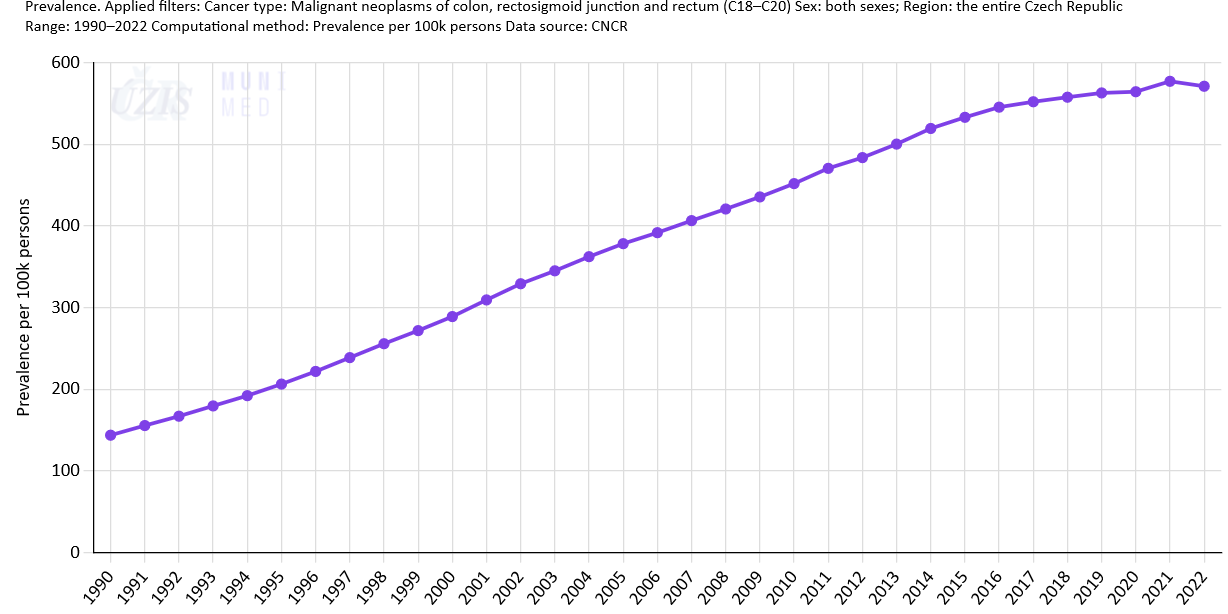
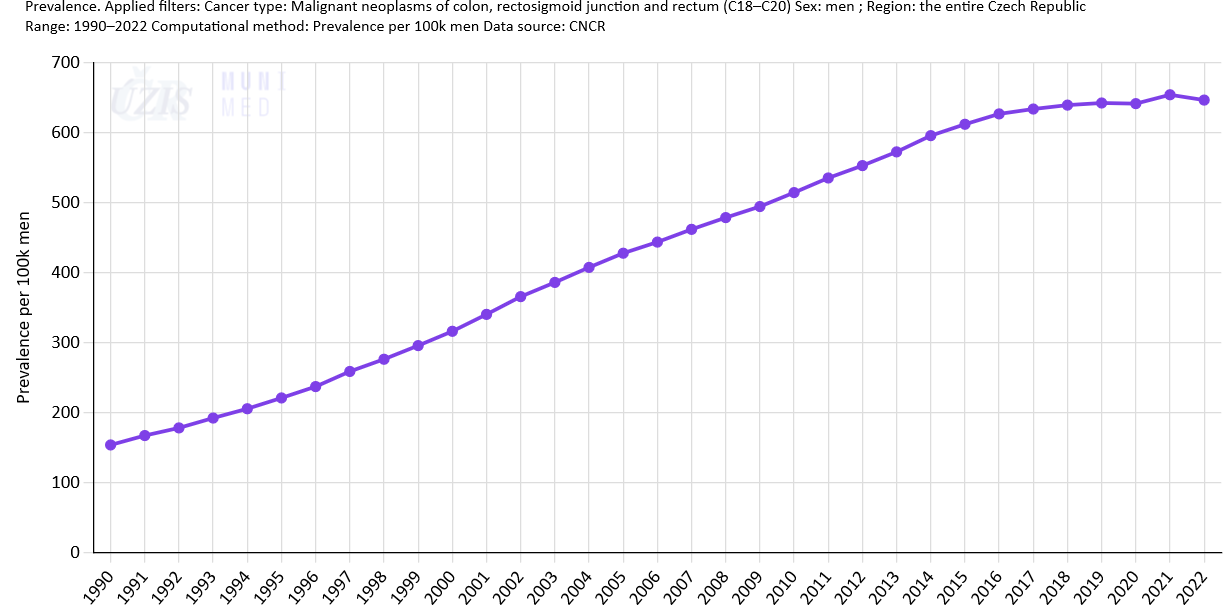
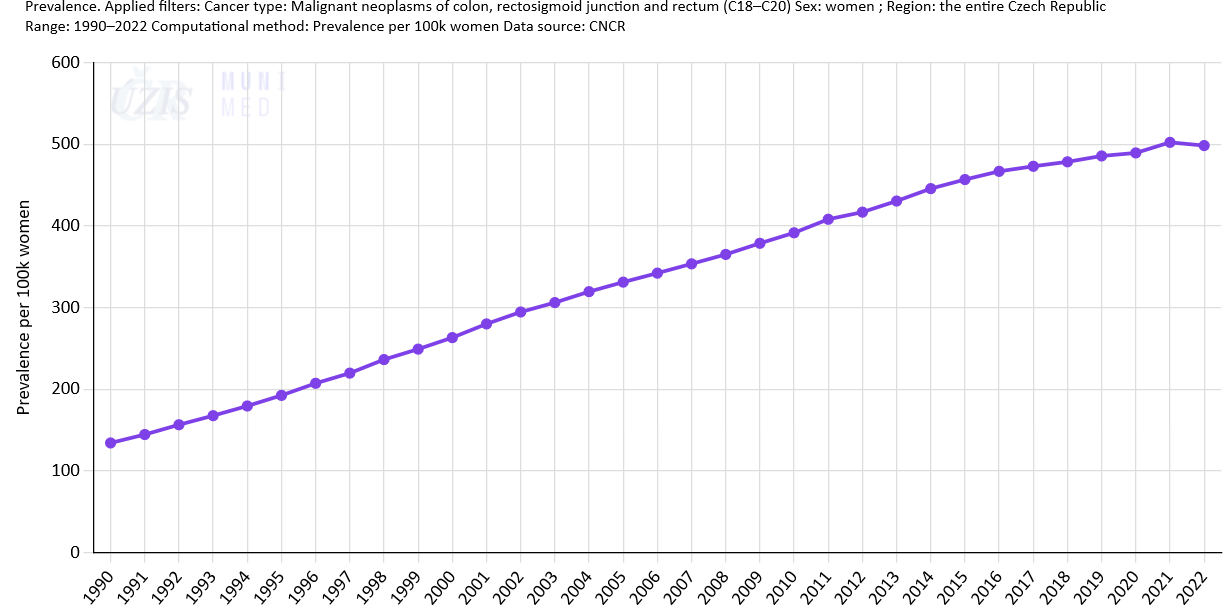
Colorectal cancer prevalence rates
Some signs of improvement have been shown in recent years: in particular, mortality rates have stabilised and even begun to decrease (see above). This trend, however, when combined with the steadily growing incidence rates, inevitably leads to an increase in prevalence rates, i.e. a higher number of colorectal cancer survivors. In 2022, the prevalence of people with a history of colorectal cancer reached 61,429 in the Czech Republic, corresponding to an almost 21% increase in comparison with 2012 (50,821 colorectal cancer survivors (Fig. 5a); the increase was more than 19% in men (Fig. 5b) and more than 22% in women (Fig. 5c).
Absolute numbers of CRC survivors
-
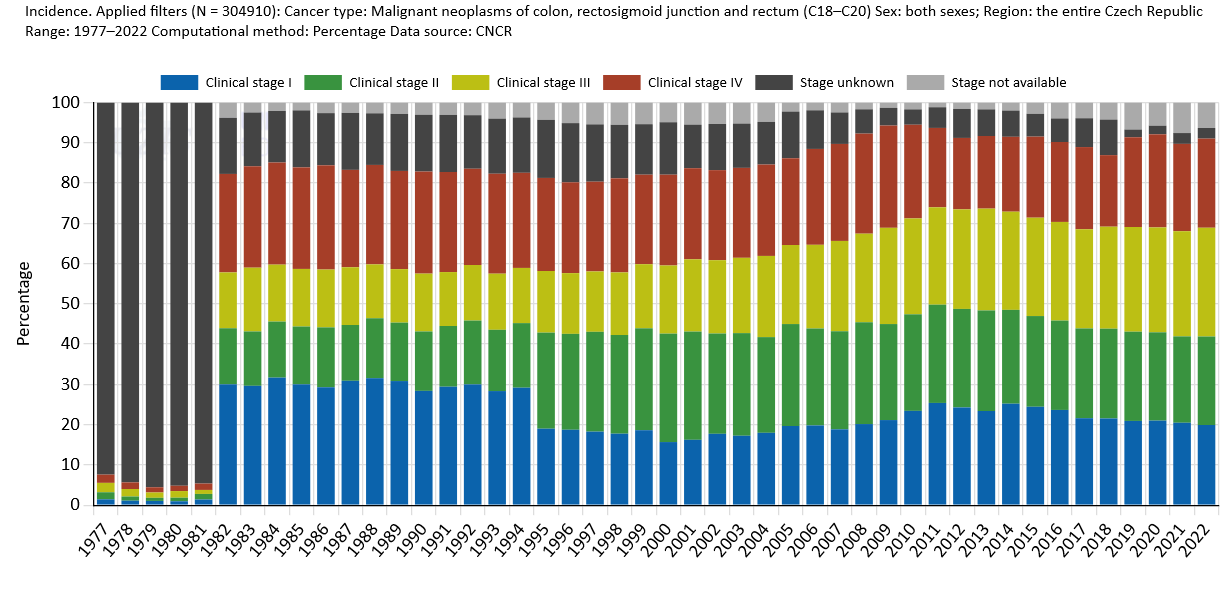
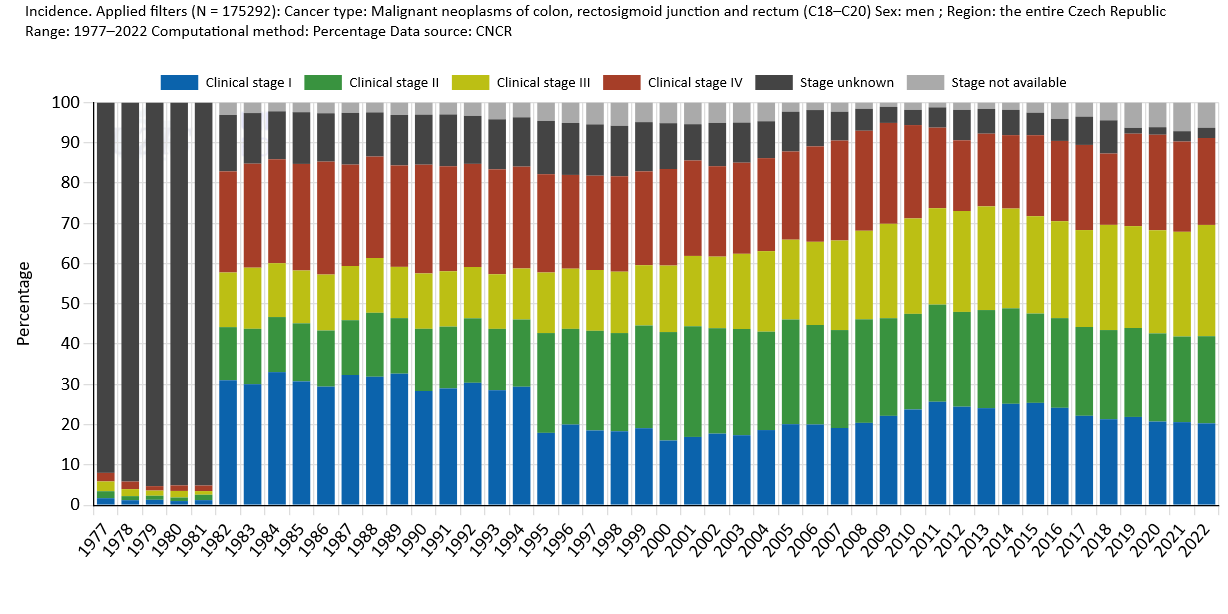
Clinical stages
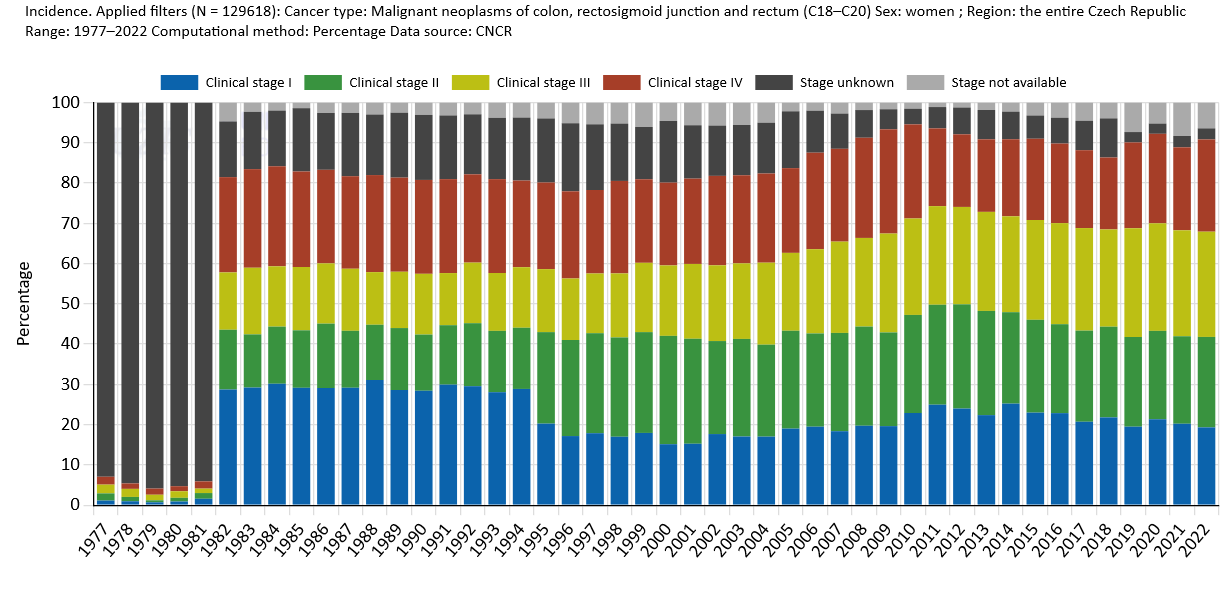
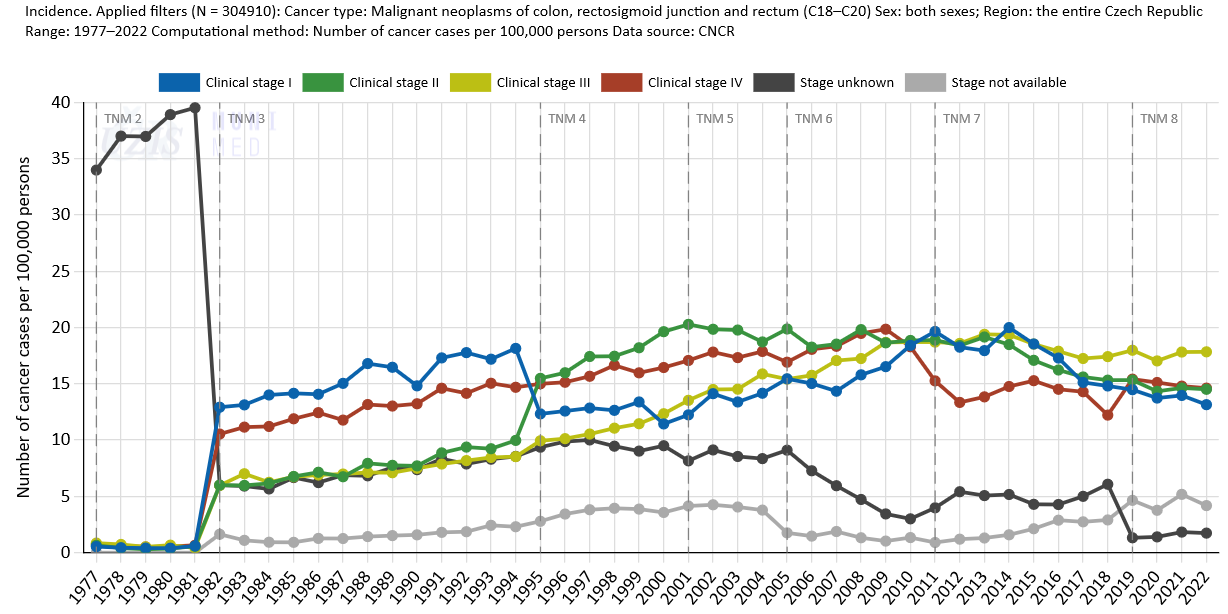
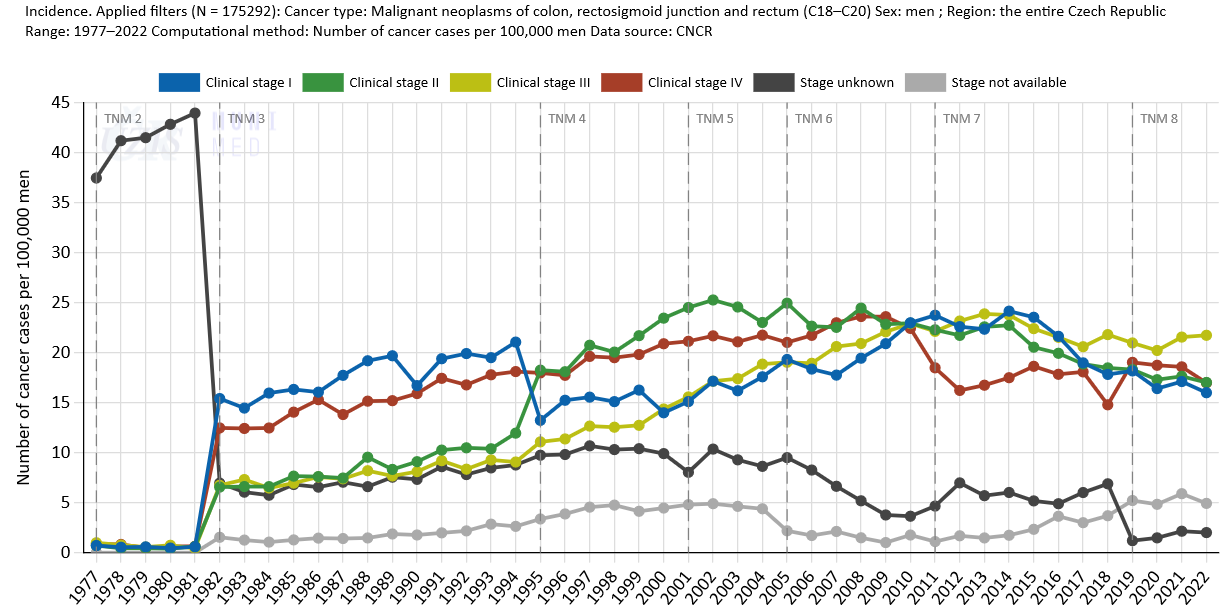
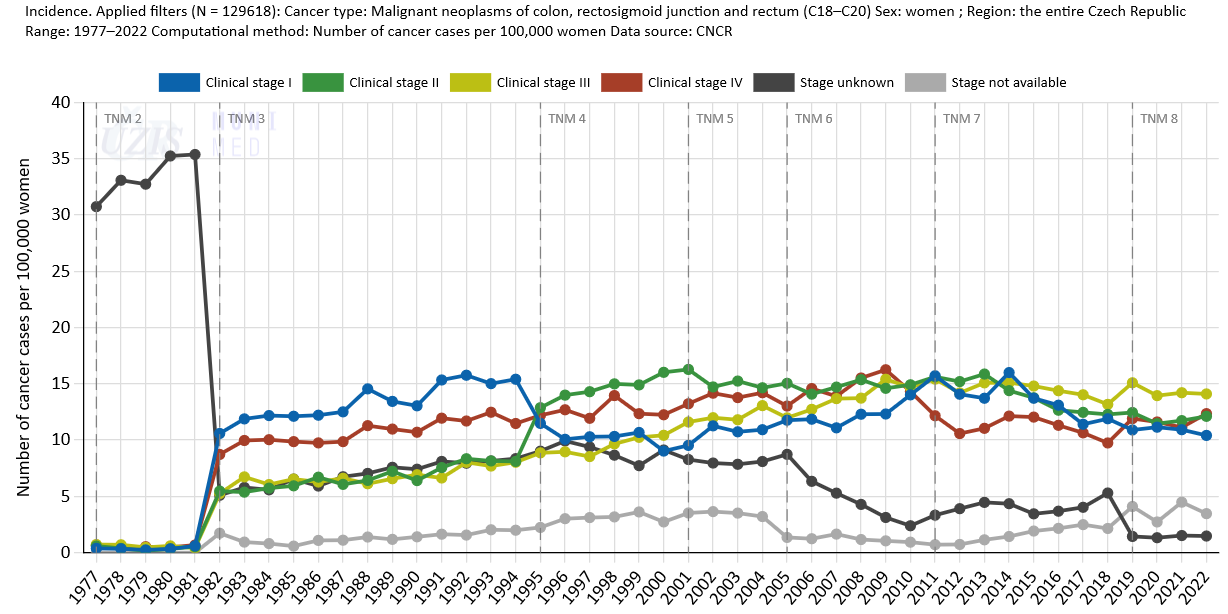
It is widely known that a cancer diagnosed at an early stage (or even at the stage of precancerous changes) is much more likely to be treated successfully and that the chance of survival in such cases is much higher. Available population-based data on colorectal cancer epidemiology in the Czech Republic, however, describes a rather gloomy situation: Figs. 7a-c show that a high proportion of new colorectal cancer patients in the Czech Republic are diagnosed with tumours in clinical stages III or IV, and that the numbers of these cases diagnosed in advanced stages are on the rise (Figs. 8a-c). This inevitably leads to markedly poorer treatment results, let alone related costs. Moreover, the situation has not much improved over time.
Proportion of clinical stages
Incidence rates according to clinical stages
-
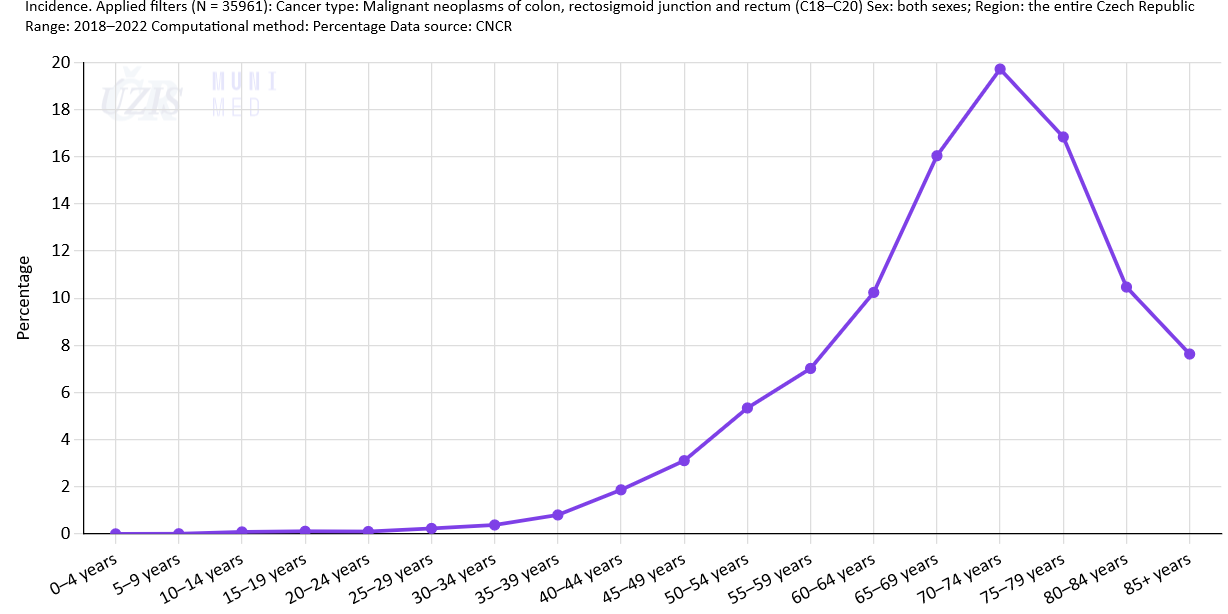
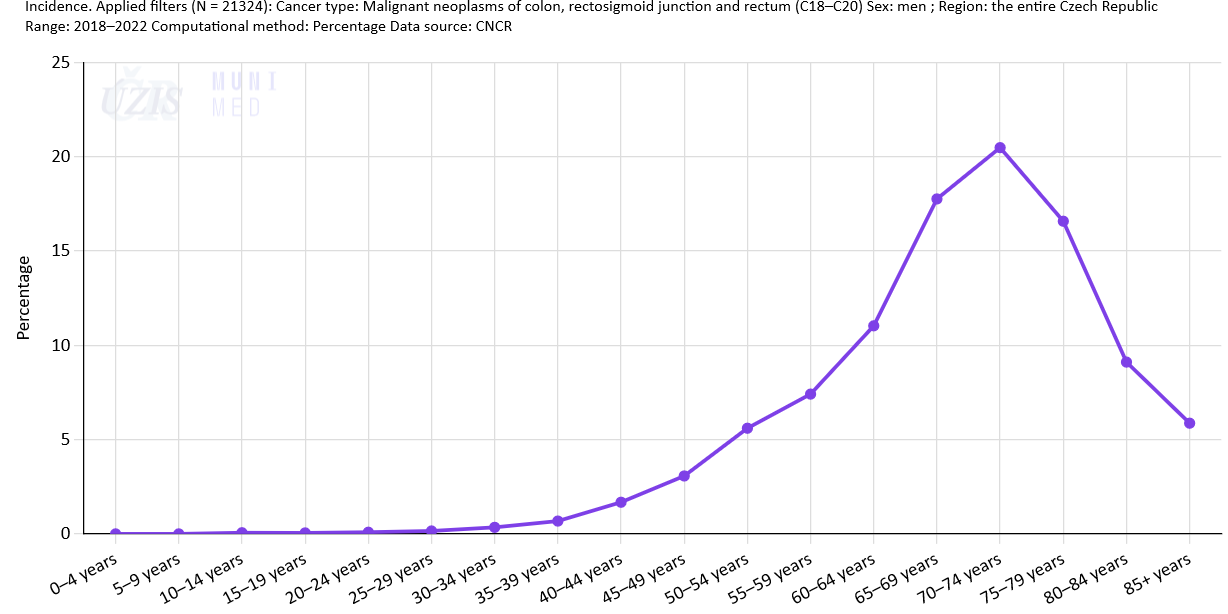
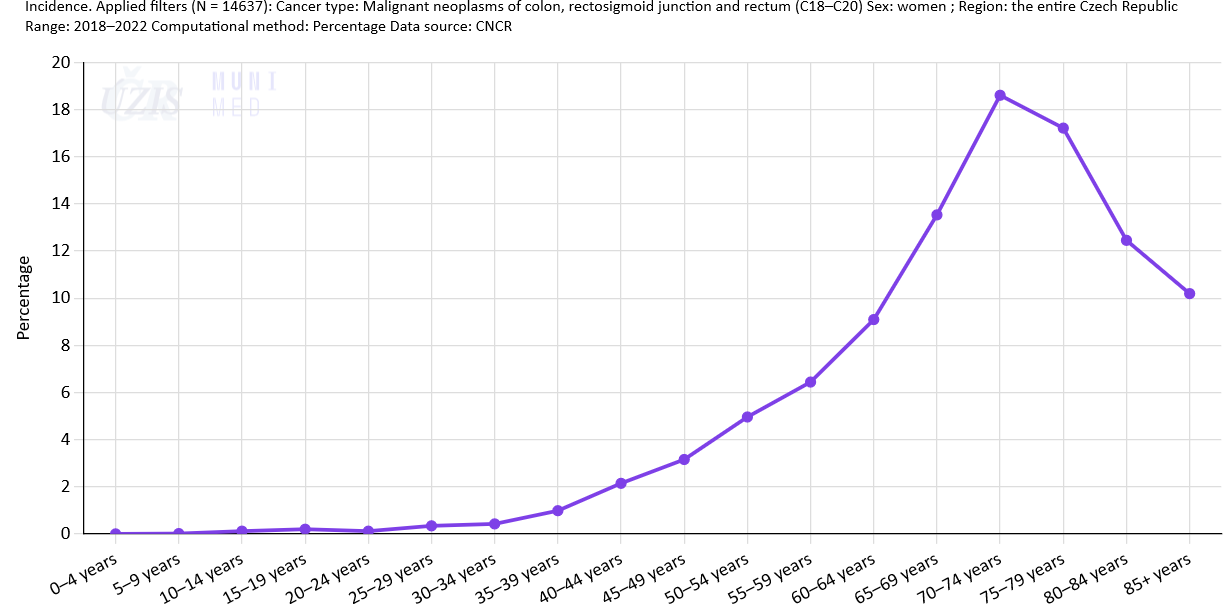
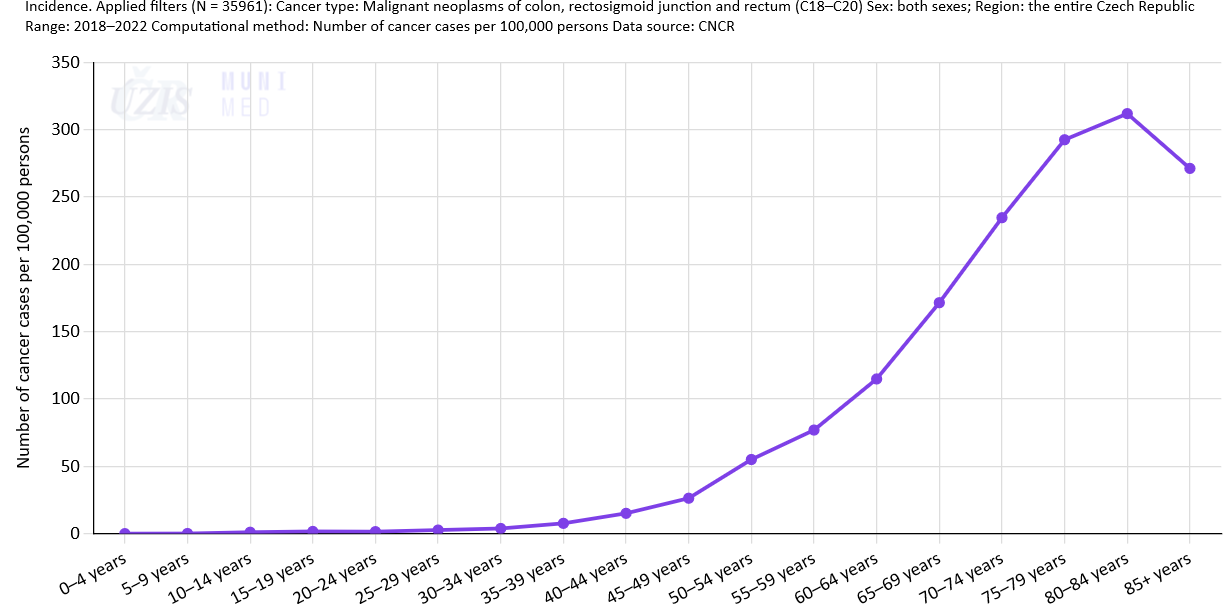
Age structure of patients
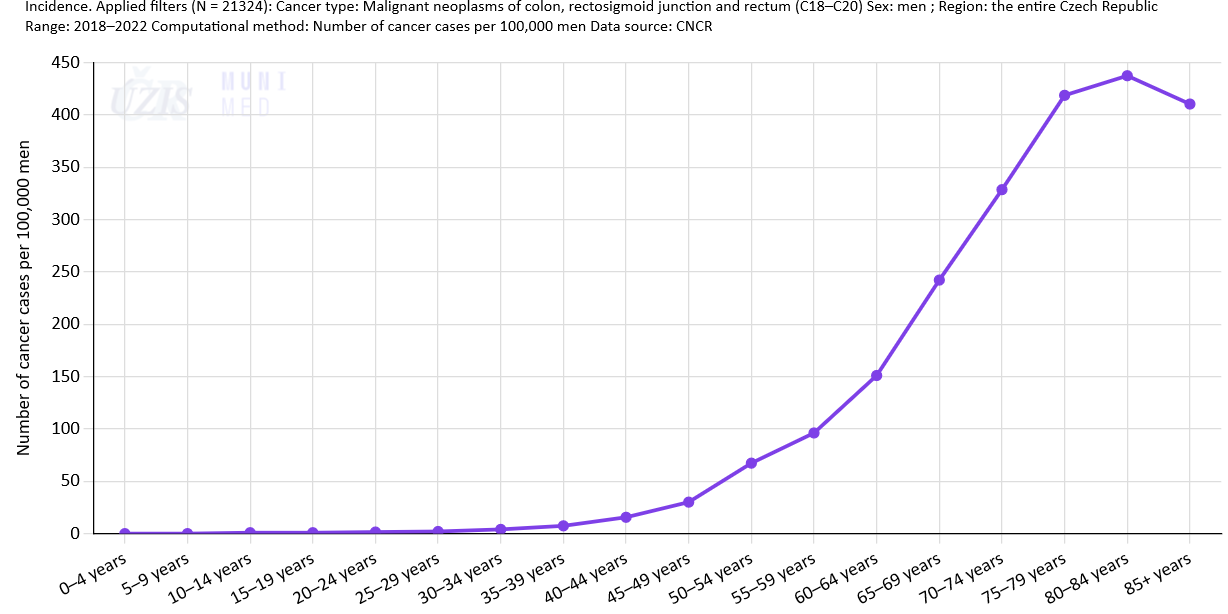
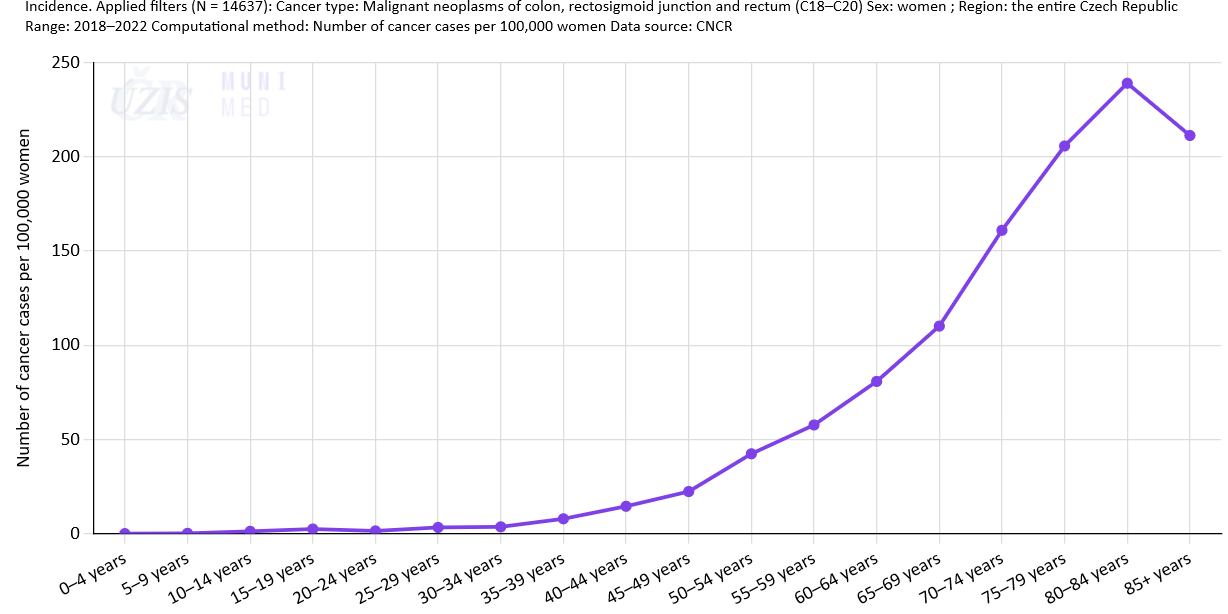
Colorectal cancer markedly affects patients in working age. The typical age of Czech colorectal cancer patients is between 65 and 79 years, but 19% of all patients are under the age of 60 (Figs. 9a-c). The profiles of age-specific incidence rates for colorectal cancer (Figs. 10a-c) demonstrate the importance of the problem that colorectal cancer presents in oldest groups of the Czech population.
Number of cases in different age categories (analysed period: 2018–2022)
-
References
- Institute of Health Information and Statistics of the Czech Republic: Czech National Cancer Registry (CNCR) [16 July 2024]. Available from WWW http://www.uzis.cz/registry-nzis/nor
- 2. Krejčí Denisa, Mužík Jan, Šnábl Ivo, Gregor Jakub, Komenda Martin, Dušek Ladislav. Portal of Cancer Epidemiology in the Czech Republic [online]. Masaryk University, Brno, 2024. [cit. 2024-07-16]. Available from: https://www.svod.cz/en/. Version 8.0.0
- Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F (2018). Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer [accessed on 21 January 2021]. Available from WWW: https://gco.iarc.fr/today.
Last updated on 16 July 2024
International comparison
Colorectal cancer (CRC) is among the most commonly diagnosed cancers worldwide. In 2020, according to the GLOBOCAN estimates [1], there were 1,931,590 new cases of CRC worldwide (3rd most common cancer worldwide, accounting for 10.7% of all cancers apart from non-melanoma skin cancer), and 519,820 new cases of CRC in Europe (2nd most common cancer in Europe, accounting for 12.9% of all cancers apart from non-melanoma skin cancer). In 2020, there were an estimated 935,173 deaths from CRC worldwide (9.5% of the total number of cancer deaths, 2nd most common cause of cancer related deaths), and 244,824 deaths from CRC in Europe (12.6% of the total number of cancer deaths, 2nd most common cause of cancer related deaths). The 5-year prevalence of CRC (i.e., the number of CRC patients who were alive five years after diagnosis) in 2020 was estimated at 5,253,335 worldwide (67.4 CRC survivors per 100,000 population) and 1,536,168 in Europe (205.1 CRC survivors per 100,000 population). In 2020, the cumulative risk of CRC in persons aged under 75 was 2.25% worldwide (2.71% in men, 1.83% in women) and 3.60% in Europe (4.50% in men, 2.85% in women) [1].
-
Basic overview of epidemiological characteristics
Tables 1 and 2 provide a basic overview of epidemiological characteristics of colorectal cancer worldwide and in Europe. This data demonstrates a significant colorectal cancer burden in European countries, which is still associated with very high mortality rates.
Table 1: Epidemiology of colorectal cancer worldwide. Source: GLOBOCAN 2020 [1].
Parameter Men Women Both sexes Incidence
number of new cases
1,065,960
865,630
1,931,590
number of new cases per 100,000 population
27.1
22.4
24.8
ASR(W)
23.4
16.2
19.5
proportion of all newly diagnosed cancers
(apart from non-melanoma skin cancer)11.4%
9.9%
10.7%
rank among all newly diagnosed cancers
(apart from non-melanoma skin cancer)3rd
2nd
3rd
Mortality
number of deaths
515,637
419,536
935,173
number of deaths per 100,000 population
13.1
10.9
12.0
ASR(W)
11.0
7.2
9.0
proportion of all cancer deaths
(apart from non-melanoma skin cancer)9.4%
9.5%
9.5%
rank among all cancer deaths
(apart from non-melanoma skin cancer)3rd
3rd
2nd
Prevalence (patients alive five years after diagnosis)
absolute number of survivors
2,850,679
2,402,656
5,253,335
rate per 100,000 population
72.5
62.2
67.4
Cumulative risk of developing colorectal cancer
from birth until the age of 75
2.71%
1.83%
2.25%
Table 2: Epidemiology of colorectal cancer in Europe. Source: GLOBOCAN 2020 [1].
Parameter Men Women Both sexes Incidence
number of new cases
281,714
238,106
519,820
number of new cases per 100,000 population
77.9
61.5
69.4
ASR(W)
37.9
24.6
30.4
proportion of all newly diagnosed cancers
(apart from non-melanoma skin cancer)13.2%
12.5%
12.9%
rank among all newly diagnosed cancers
(apart from non-melanoma skin cancer)3rd
2nd
2nd
Mortality
number of deaths
131,885
112,939
244,824
number of deaths per 100,000 population
36.5
29.2
32.7
ASR(W)
16.1
9.5
12.3
proportion of all cancer deaths
(apart from non-melanoma skin cancer)12.3%
13.0%
12.6%
rank among all cancer deaths
(apart from non-melanoma skin cancer)2nd
3rd
2nd
Prevalence (patients alive five years after diagnosis)
absolute number of survivors
822,371
713,797
1,536,168
rate per 100,000 population
227.4
184.4
205.1
Cumulative risk of developing colorectal cancer
from birth until the age of 75
4.50%
2.85%
3.60%
-
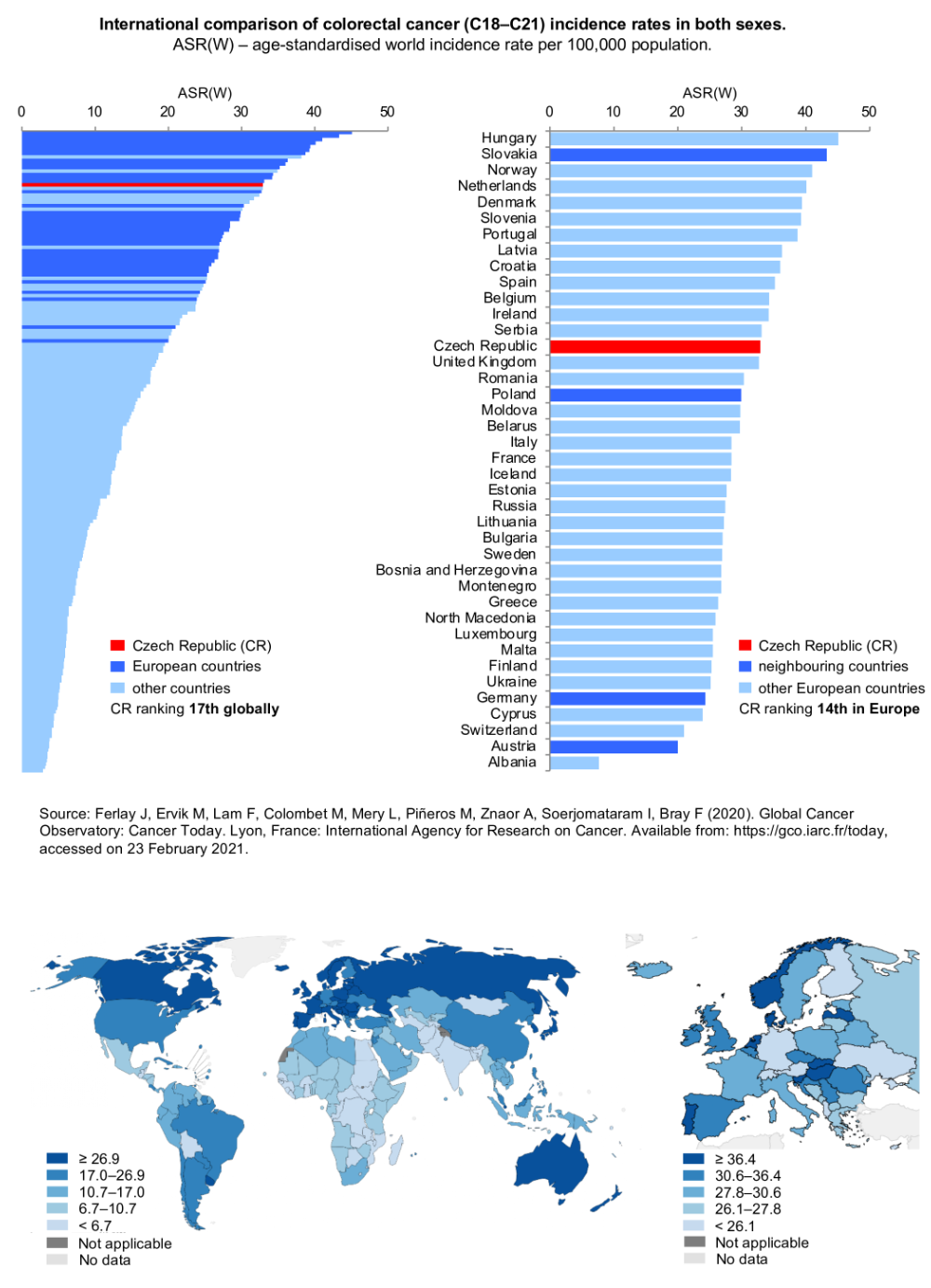
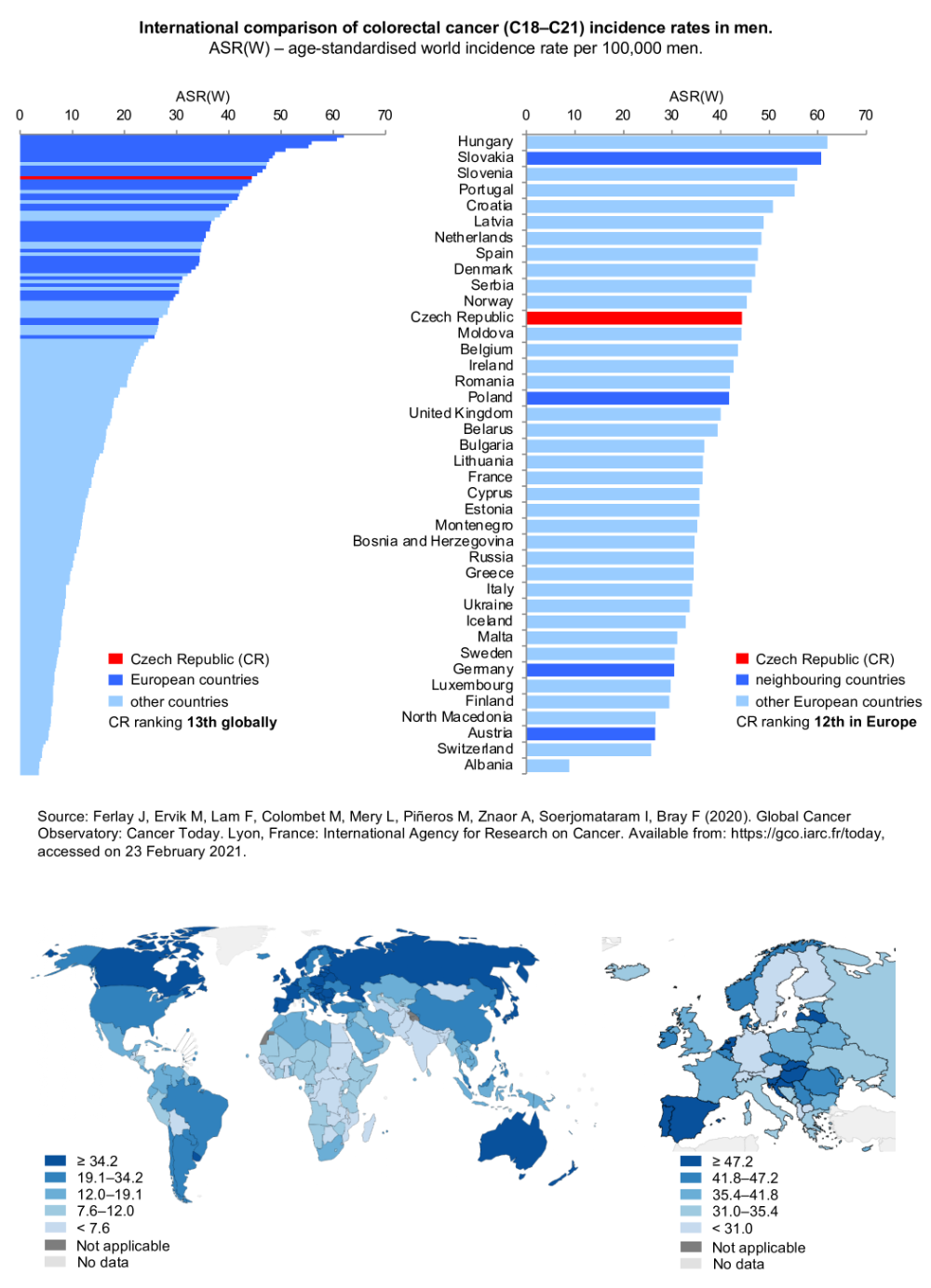
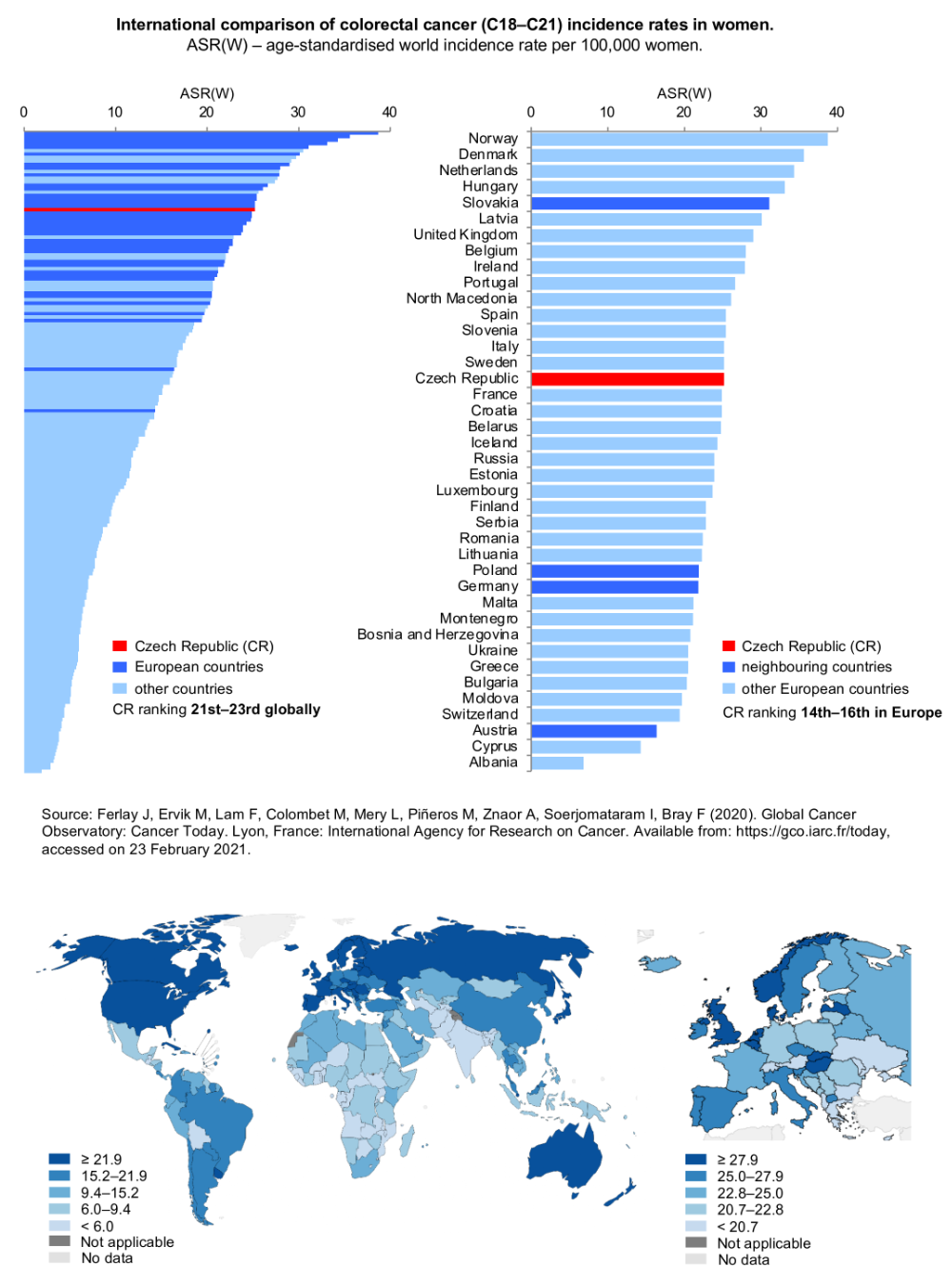
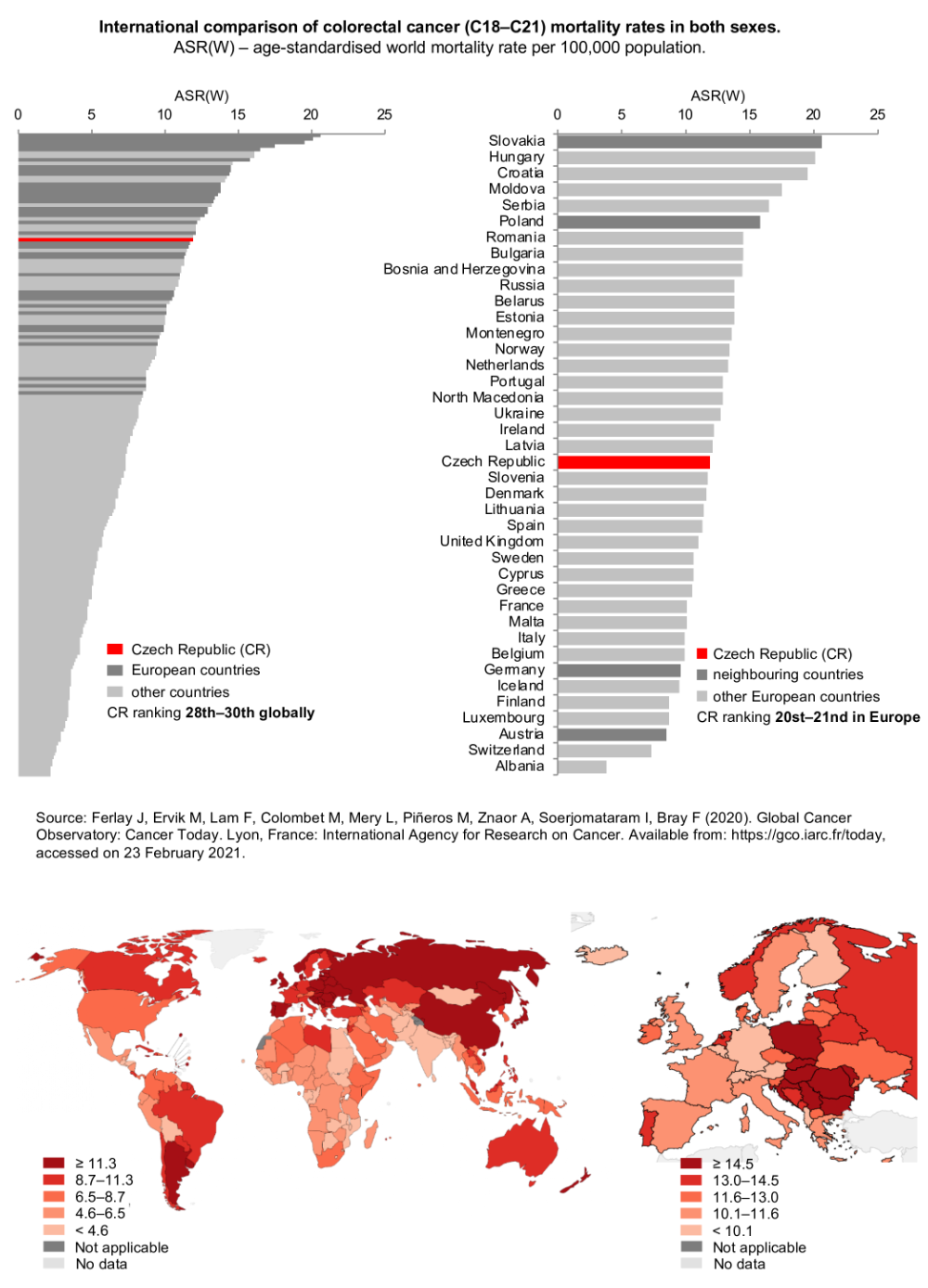
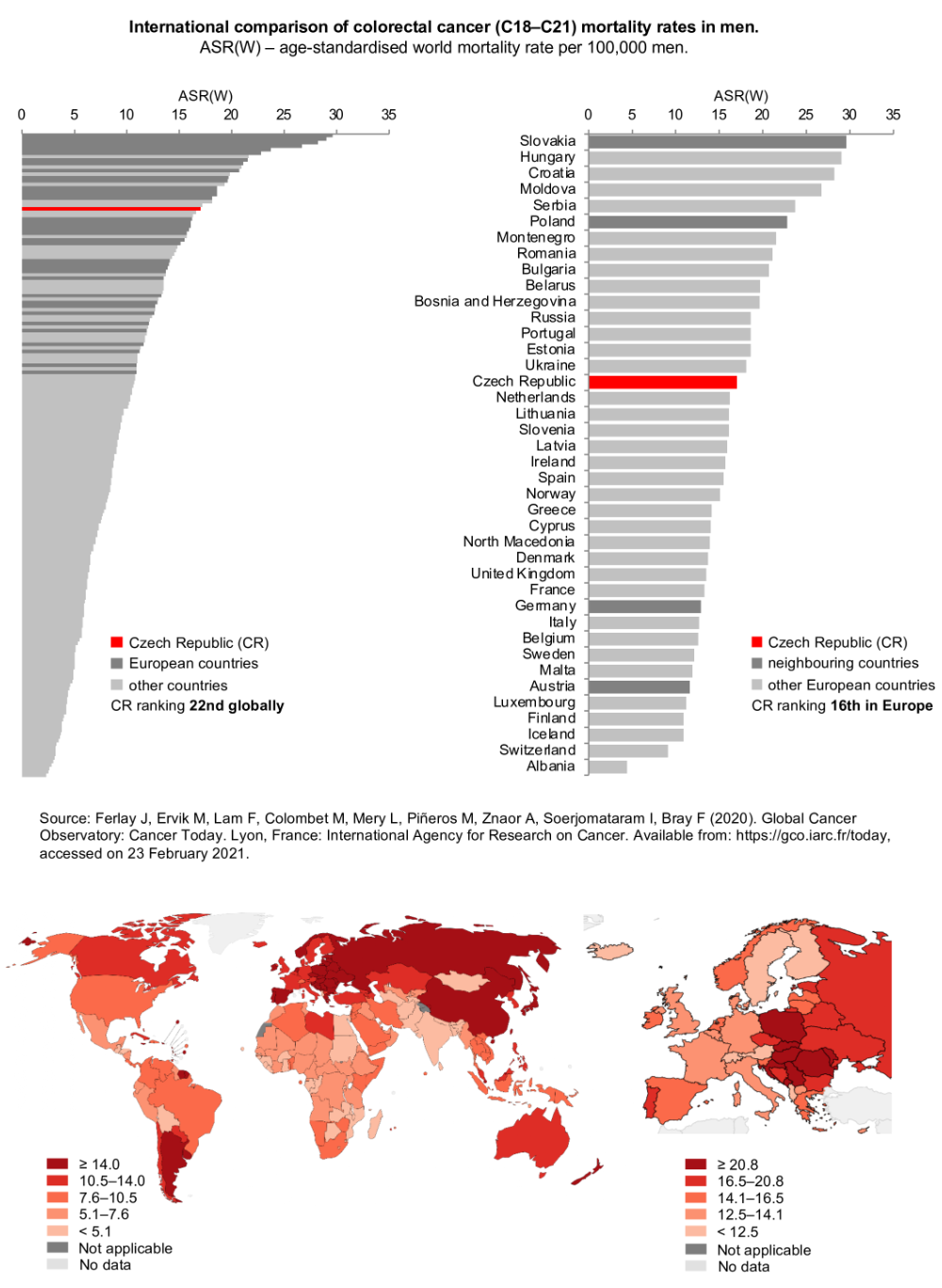
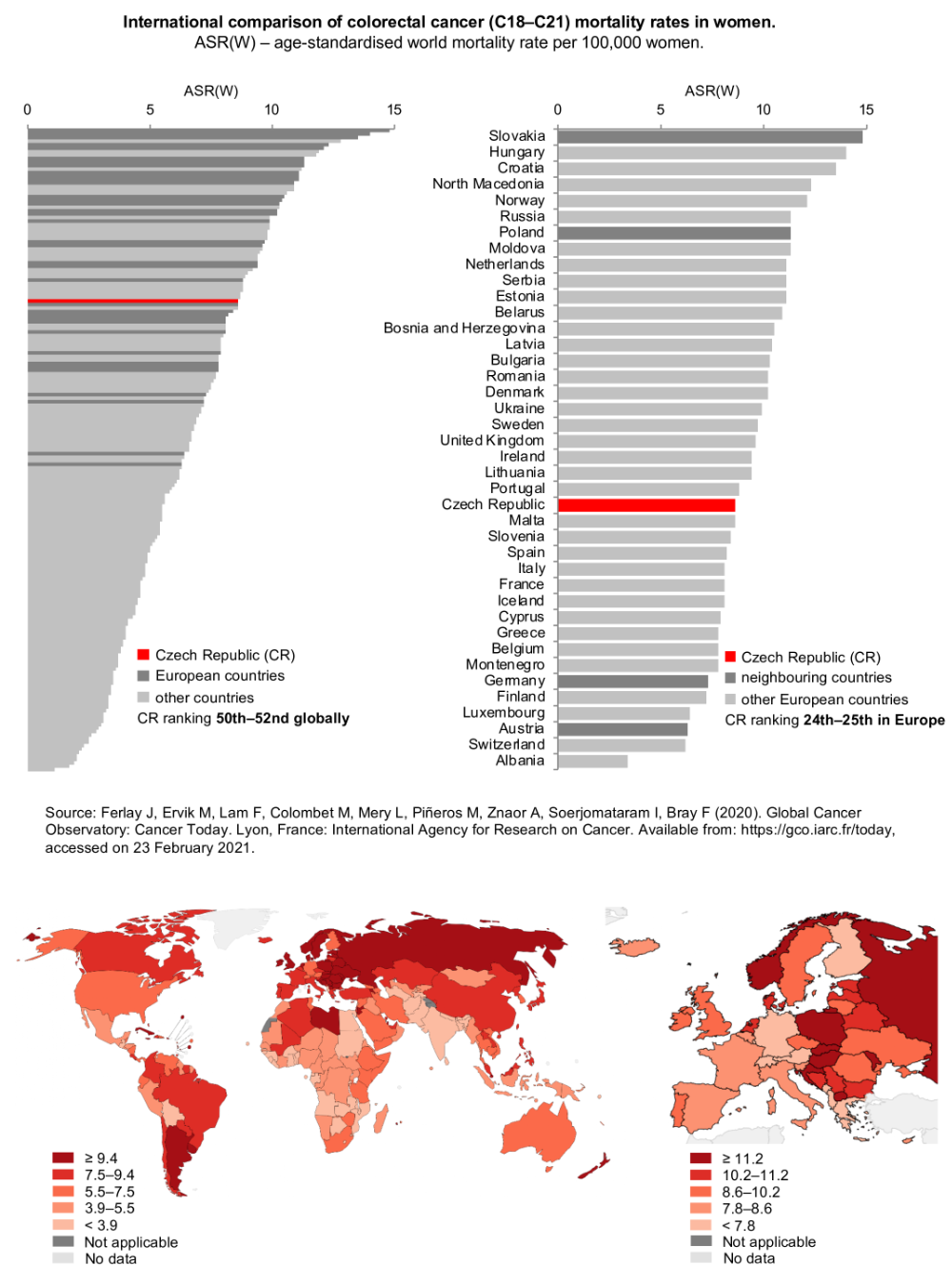
Incidence and mortality
High colorectal cancer incidence and mortality rates are also shown in Figures 1 and 2. Recent statistics have indicated that the burden of colorectal cancer in the Czech Republic is above the global average, and this applies particularly to Czech men. Czech colorectal cancer incidence rates in men rank 13th worldwide and 12th in Europe, while women’s rates rank 21st–23rd worldwide and 14th–16th in Europe. From the global perspective, colorectal cancer incidence and mortality rates have continuously been highest in Central and West European countries. Among European countries in 2020, Hungary, Slovakia and Norway had the highest incidence rates of colorectal cancer; the Czech Republic ranked 14th.
Figure 1a: International comparison of colorectal cancer incidence rates – both sexes. ASR(W) – age-standardized world incidence rate per 100,000 population. Data source: GLOBOCAN 2020
Figure 1b: International comparison of colorectal cancer incidence rates – men. ASR(W) – age-standardized world incidence rate per 100,000 population. Data source: GLOBOCAN 2020
Figure 2a: International comparison of colorectal cancer mortality rates – both sexes. ASR(W) – age-standardized world mortality rate per 100,000 population. Data source: GLOBOCAN 2020
Figure 2b: International comparison of colorectal cancer mortality rates – men. Data source: GLOBOCAN 2020
-
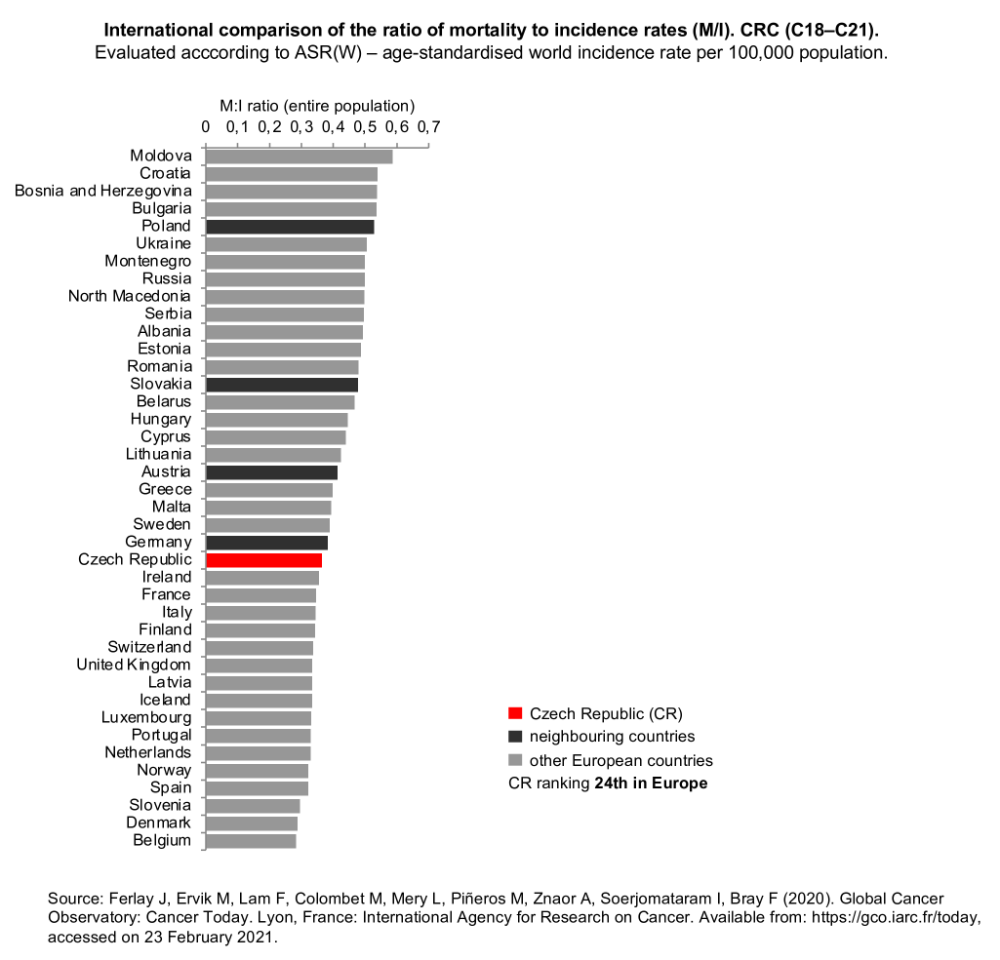
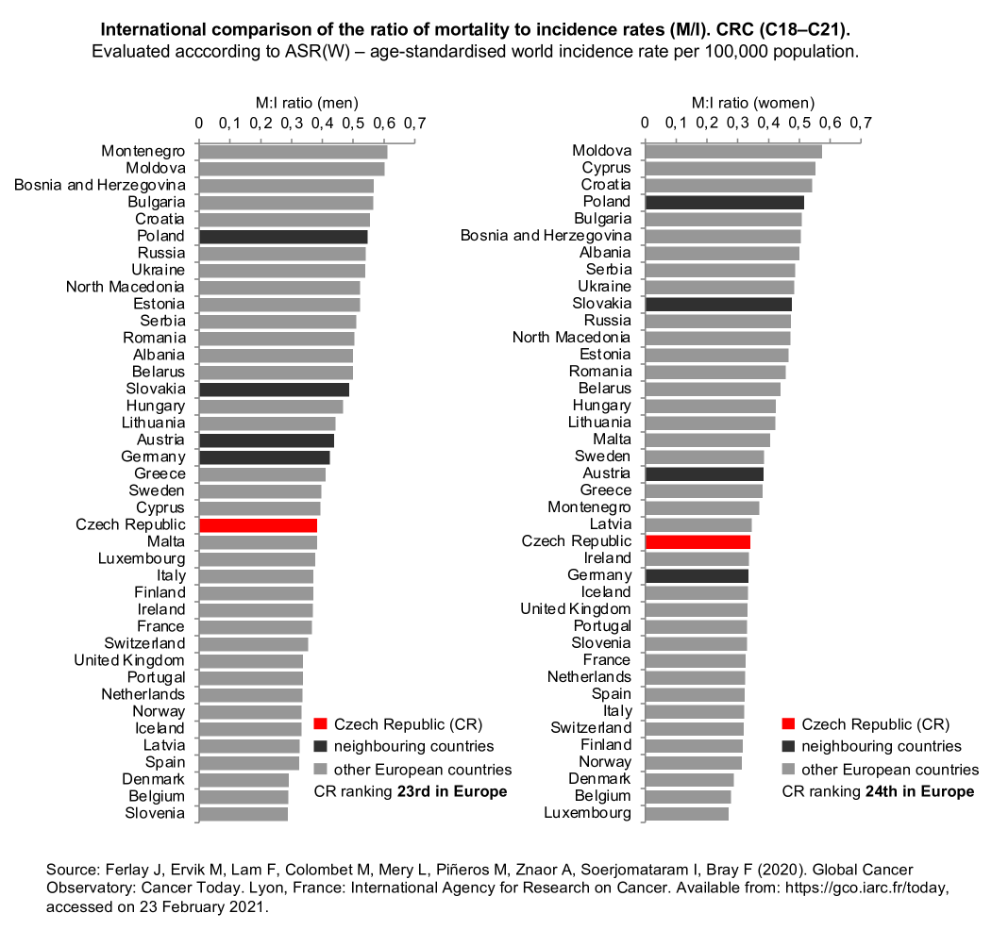
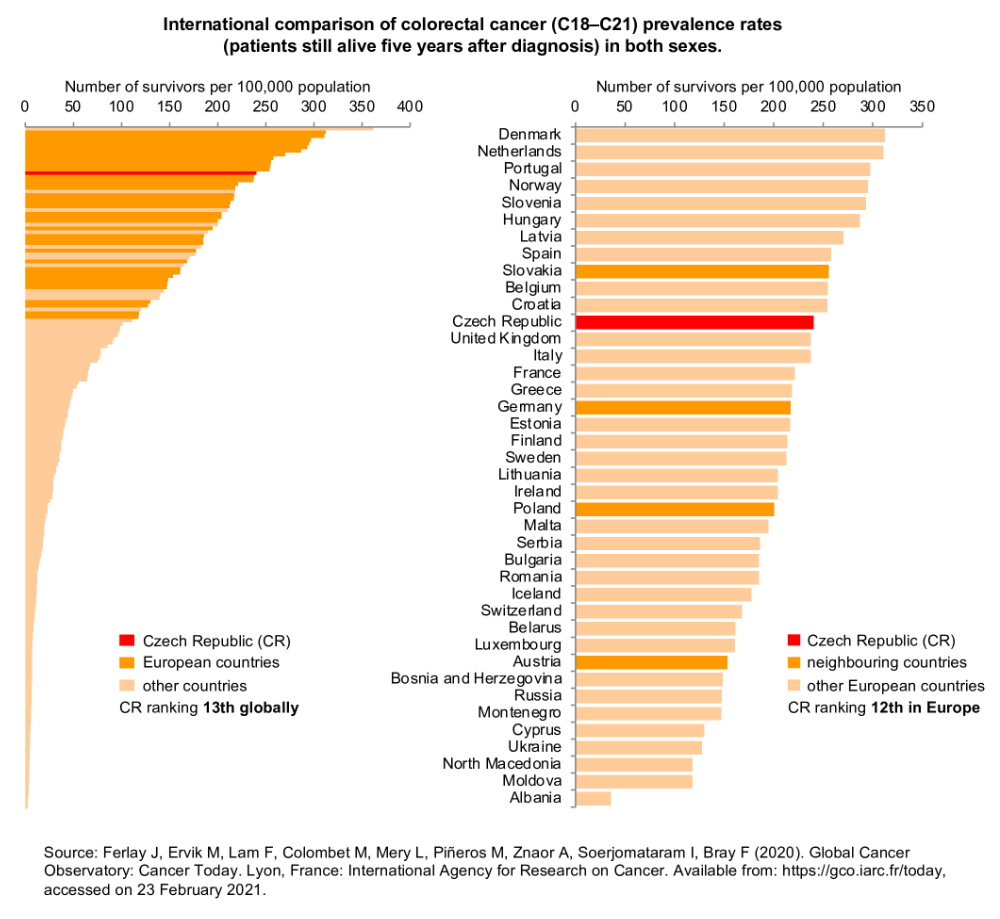
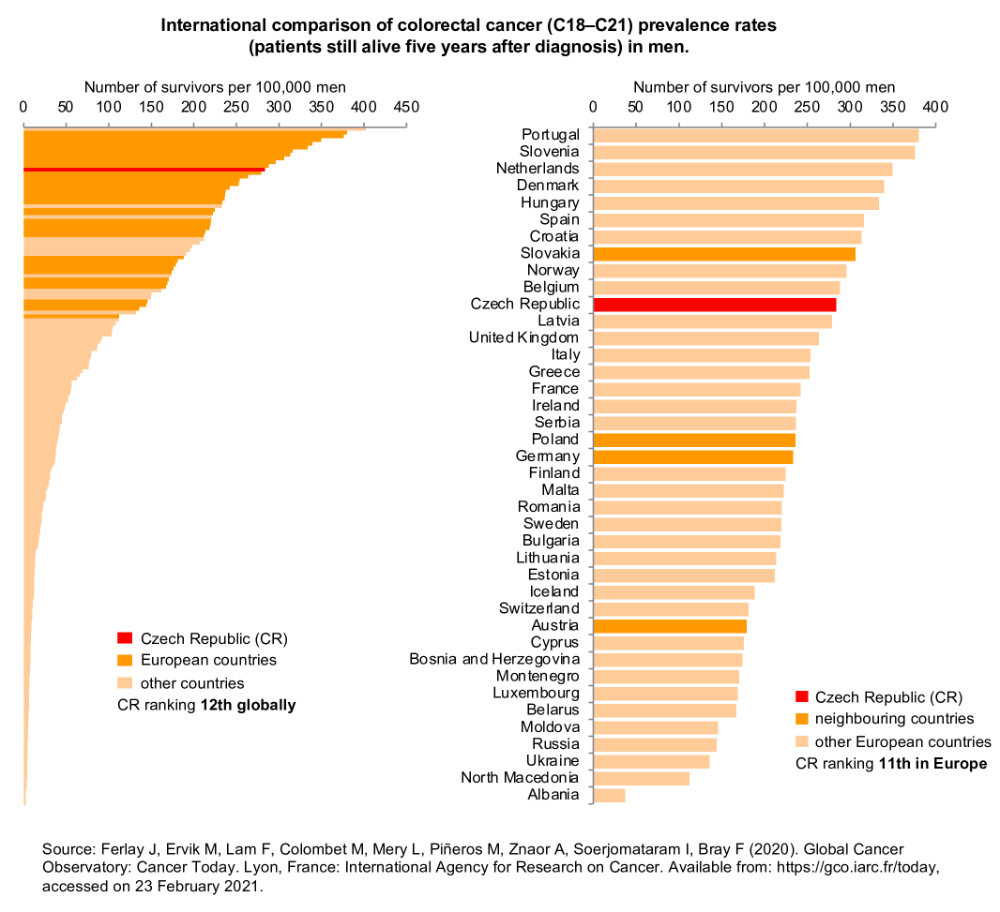
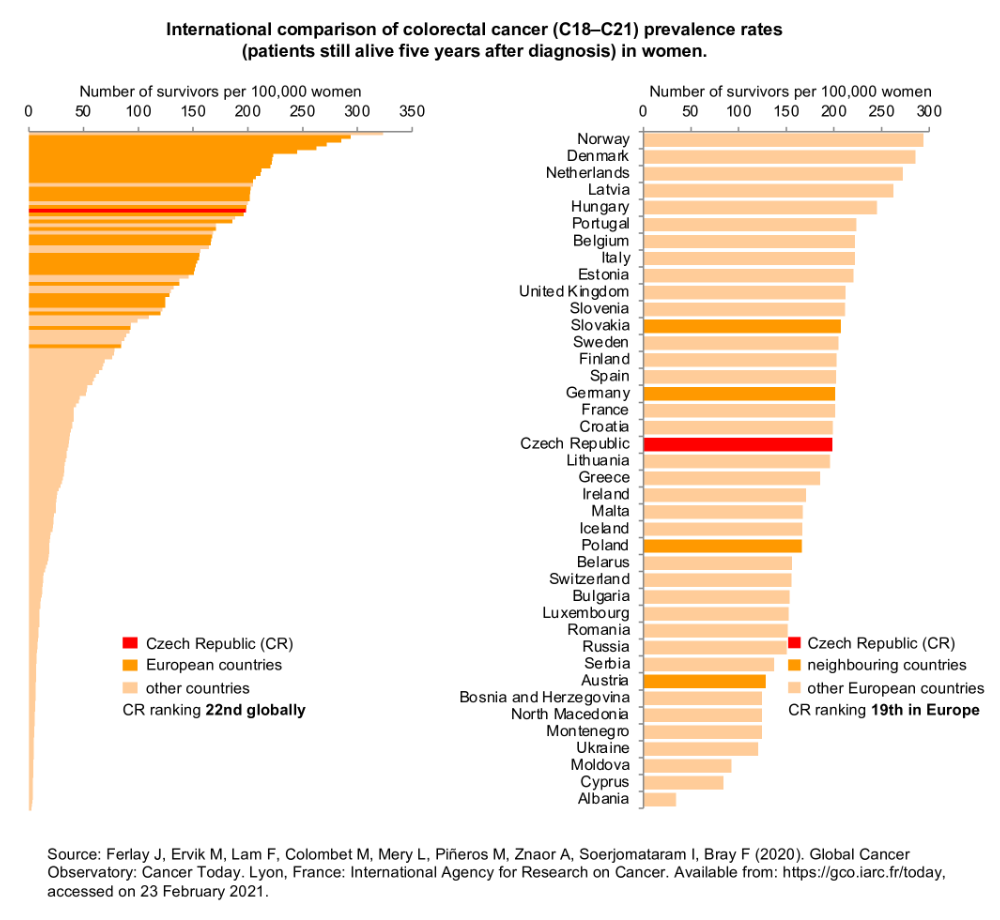
Prevalence and M/I ratio
International epidemiological statistics make it possible to estimate the ratio of mortality to incidence rates (M/I), which can be considered as an indirect indicator of survival of colorectal cancer patients in a given country (Figure 3). According to the most recent statistics, the Czech Republic with its M/I ratio at 0.37 slowly approaches the developed Western European countries, for which the M/I ratio ranges from 0.27 to 0.39. Recent data from the Czech National Cancer Registry [2] correspond to a M/I ratio close to 0.4: the incidence of 31.63 and the mortality of 13.13 (data from 2018 recalculated as ASR-W) give the ratio of 0.42. Internationally assessed prevalence rates (i.e., number of patients alive five years after diagnosis) are shown in Figure 4. As a logical consequence, the highest prevalence rates have been reported for countries with the lowest values of M/I ratio. As for colorectal cancer prevalence rates, the Czech Republic is slightly above-average among European countries.
Figure 3a: International comparison of the ratio of mortality to incidence rates (M/I) – both sexes. Evaluation was done using the ASR(W) – age-standardized world incidence rate per 100,000 population. Data source: GLOBOCAN 2020
Figure 4a: International comparison of prevalence rates (patients alive five years after diagnosis) – both sexes. Data source: GLOBOCAN 2020
Figure 4b: International comparison of prevalence rates (patients alive five years after diagnosis) – men. Data source: GLOBOCAN 2020
-
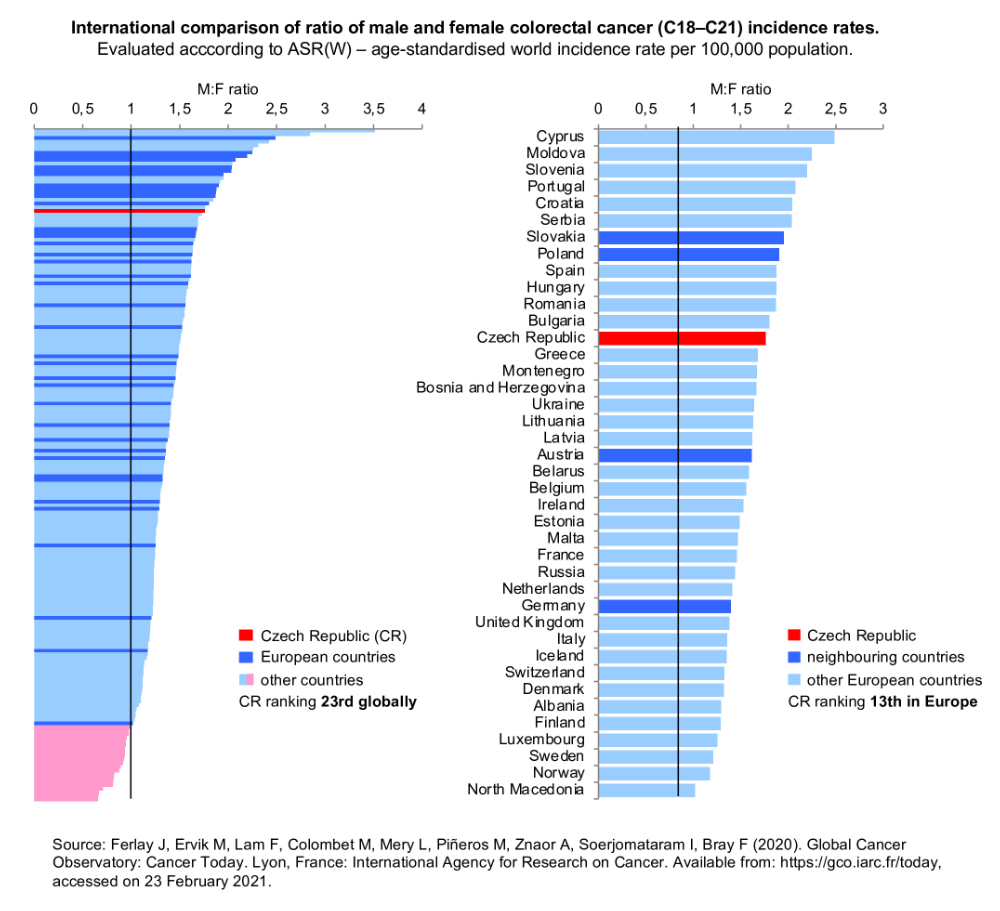
Ratio of CRC incidence rates in men and women
International statistics have also confirmed that men have higher colorectal cancer incidence rates than women. The men:women ratio in the Czech population is 1.76, which ranks 13th in Europe (Figure 5). High values of this index are typical for Central European populations, while Nordic countries have reported lower ratios (typically less than 1.40).
-
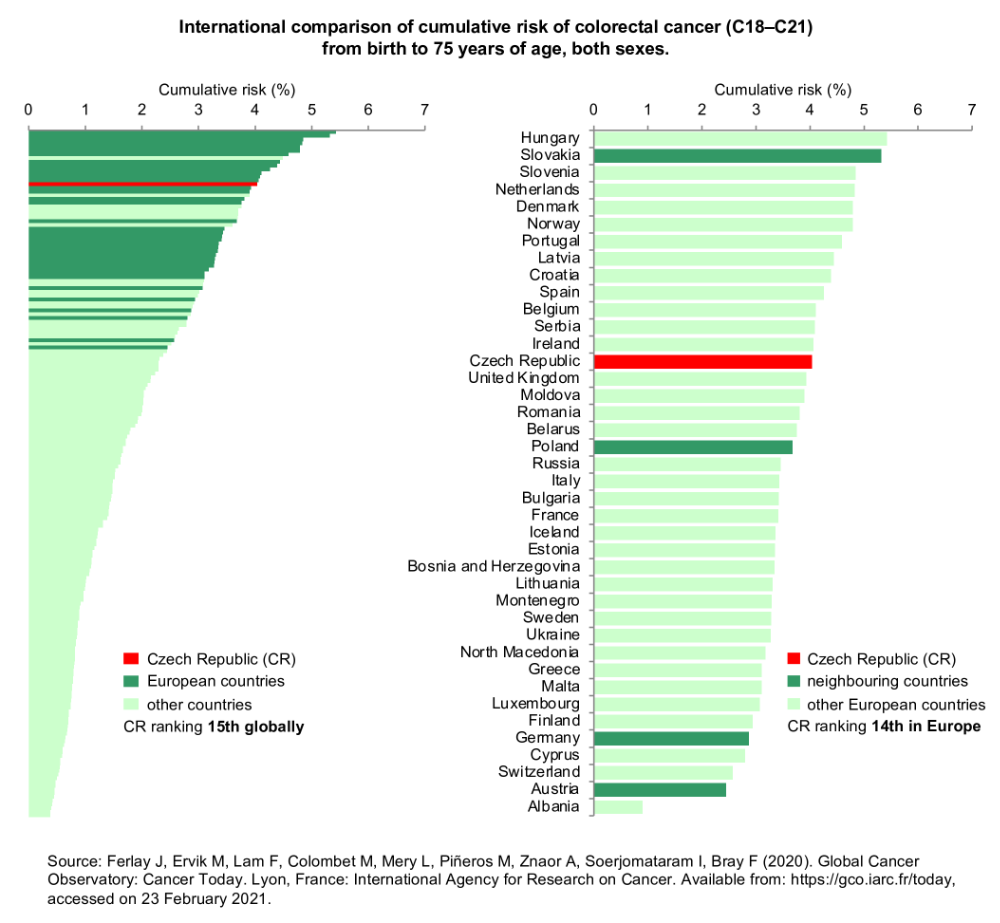
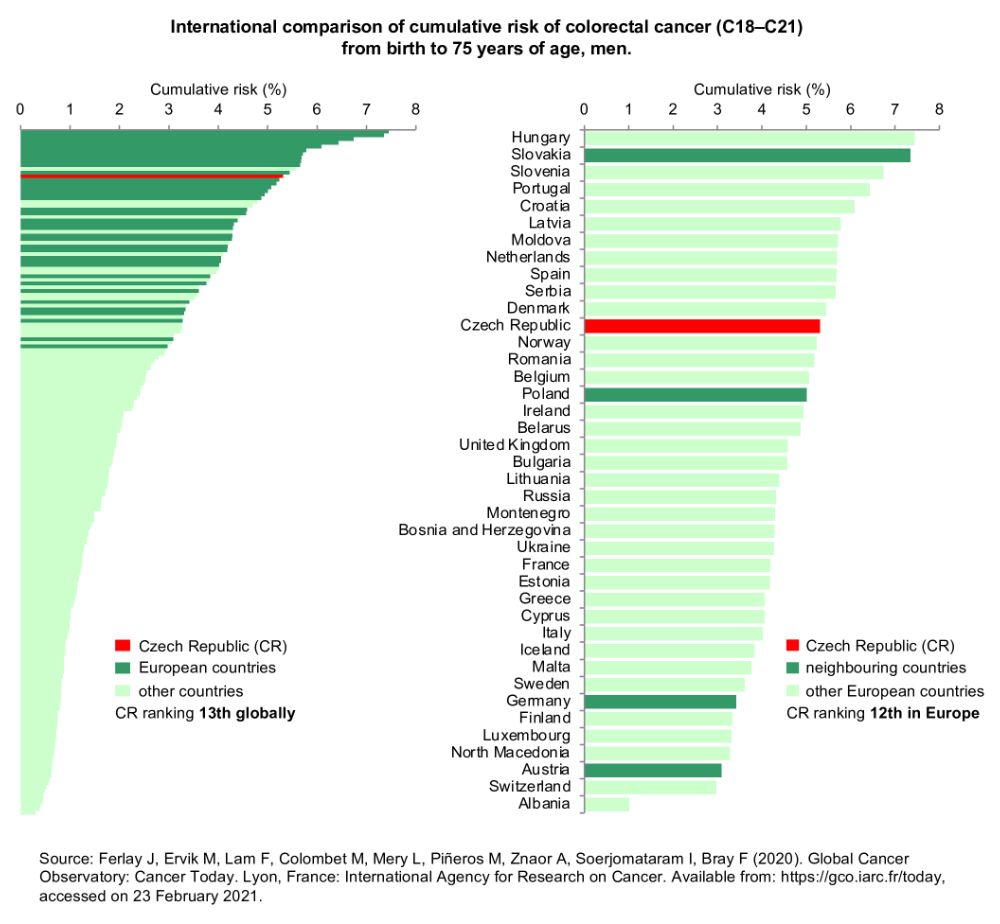
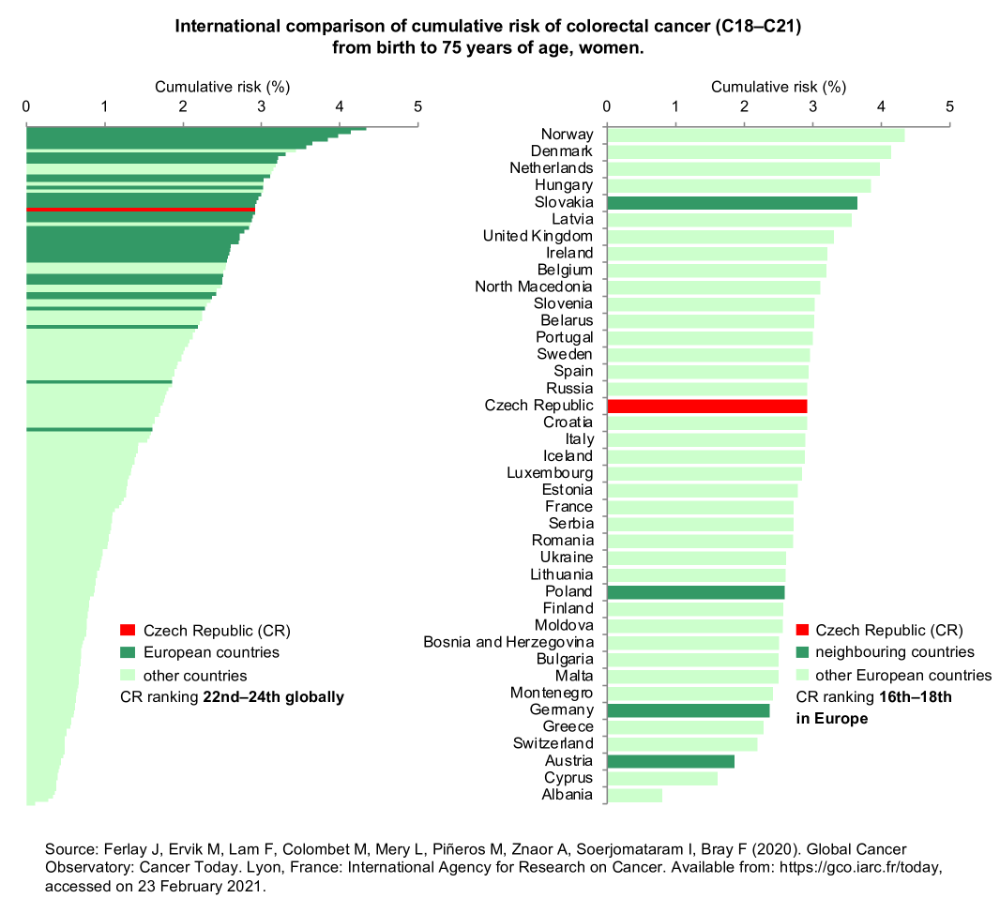
Cumulative risk
Let us conclude this overview of international statistics with a summary of cumulative risk of colorectal cancer from birth until the age of 75 (Figure 6). High values of this risk reflect a high population burden with this disease, which is typical for European countries in particular. Cumulative risk for the Czech Republic is 4.04, so the Czech population ranks 15th globally and 14th in Europe.
Figure 6a: International comparison of cumulative risk of colorectal cancer from birth to 75 years of age – both sexes. Data source: GLOBOCAN 2020
Figure 6b: International comparison of cumulative risk of colorectal cancer from birth to 75 years of age – men. Data source: GLOBOCAN 2020
-
References
- Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F (2018). Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer [accessed on 1 March 2021]. Available from WWW: https://gco.iarc.fr/today.
- Dušek L., Mužík J., Kubásek M., Koptíková J., Žaloudík J., Vyzula R. Epidemiology of malignant tumours in the Czech Republic [online]. Masaryk University, Brno (Czech Republic) [2005], [accessed on 1 March 2021]. Available from WWW: http://www.svod.cz. Version 7.0 [2007], ISSN 1802-8861.
Last updated on 1 March 2021